Symmetry and SBRT for Stage 1A NSCLC
Summary
| Institution: | Location: |
| The Prince of Wales Hospital | Randwick, NSW Australia |
| Patient: | Diagnosis: |
| 75-year-old Male | T1aN0M0, Stage 1A non-small cell lung carcinoma (NSCLC) of the left upper lobe of the lung |
| Plan: | Authors: |
| 54Gy to the 95% isodose to cover PTV, 18Gy x 3 fractions | Dr. Wenchang Wong, Radiation Oncologist Simon Downes, Chief Physicist Dr. Stéphanie Corde, Deputy Chief Physicist Lyn Emanuel, Senior Radiation Therapist Sandra Rayner, Senior Radiation Therapist Kylie Miller, Radiation Therapist And the rest of the POWH Radiation Oncology staff |
Patient history and diagnosis
This patient had significant medical co-morbidities with ischaemic heart disease requiring coronary artery by-pass graft a few years earlier, type II non-insulin dependent diabetes mellitus, chronic obstructive pulmonary disease, peripheral vascular disease with leg claudication at 100 meters, chronic renal failure, peripheral neuropathy and arterial foot ulcer. He was a smoker with a 50 pack per year history.
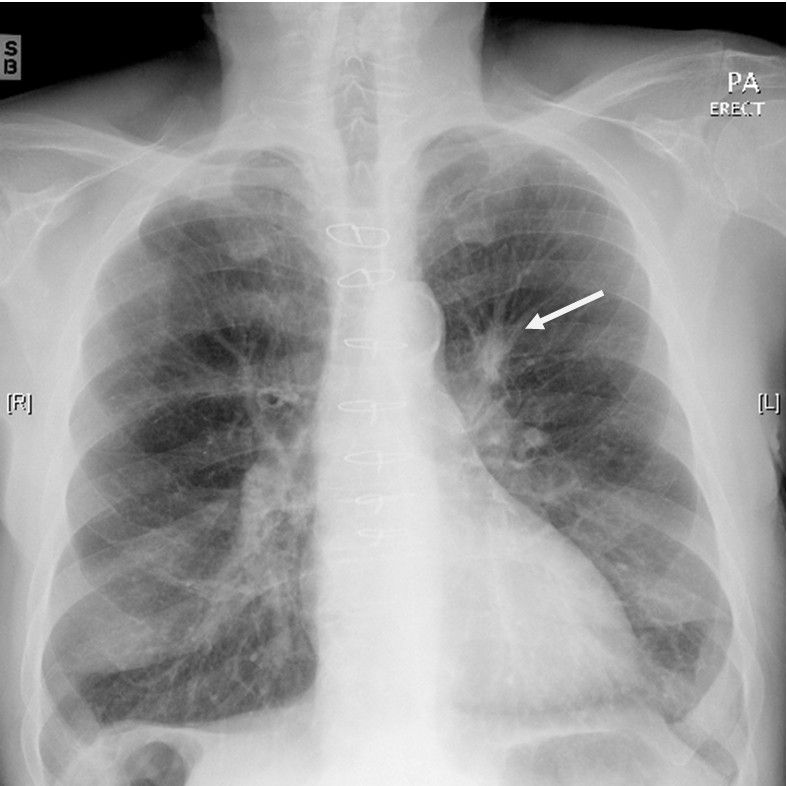
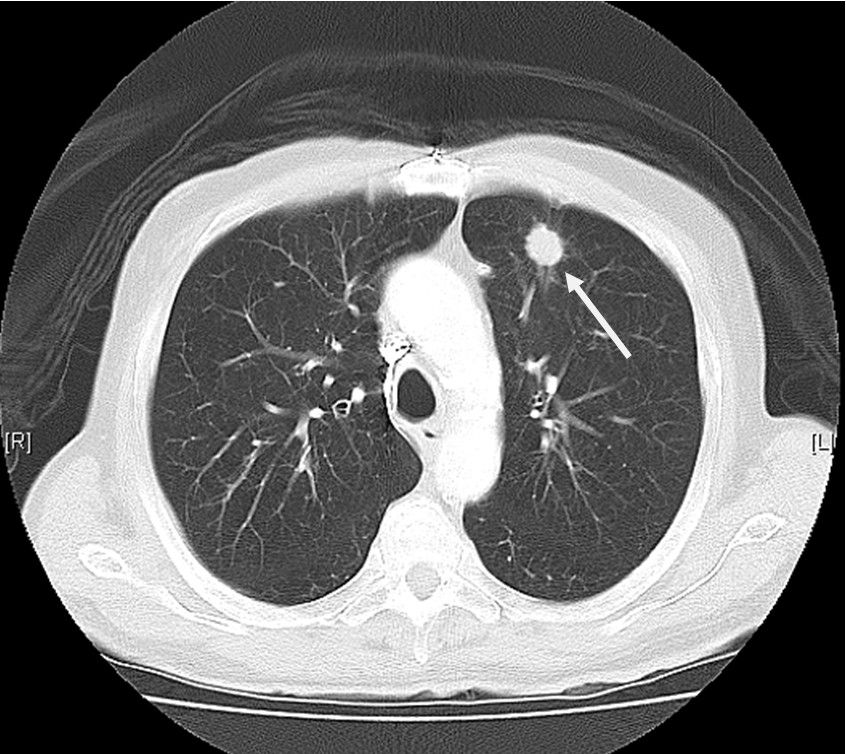
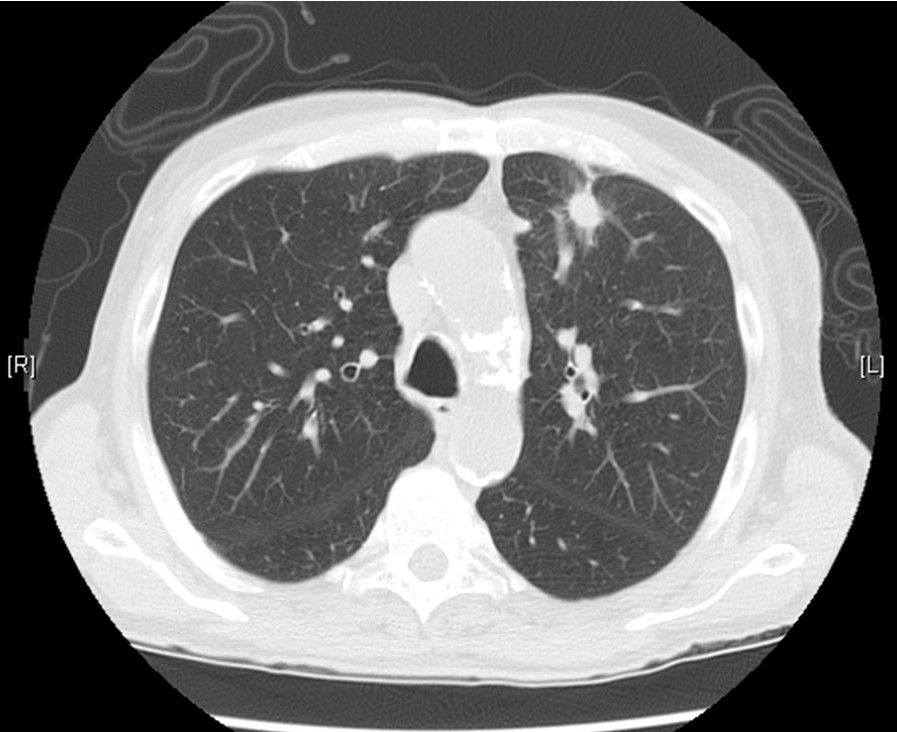
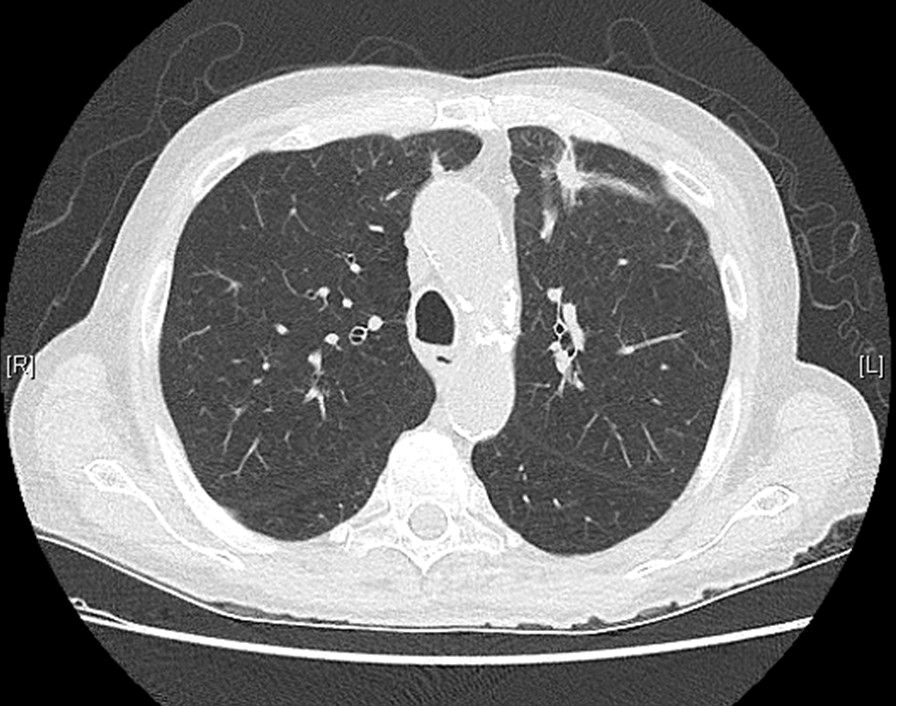
He was admitted to hospital with a short history of cough and exertional dyspnoea. A cardiac cause of his symptoms was excluded after extensive investigations but a chest X-ray showed an irregular mass in the left upper lobe of the lung. A CT scan of the chest confirmed a 17mm spiculated mass in the anterior aspect of the left upper lobe. There were no enlarged lymph nodes or other lung lesions. A fine needle aspiration biopsy of the lesion confirmed adenocarcinoma consistent with primary lung origin. A staging PET/CT scan showed abnormal glucose metabolism in the primary lesion only with no evidence of regional or widespread disease. Final stage was T1aN0M0, Stage 1A non-small cell lung carcinoma (NSCLC) of the left upper lobe of the lung. As this patient was not a surgical candidate, it was decided to treat him curatively with Stereotactic Body Radiotherapy (SBRT) to 54 Gy in 3 fractions over one week.
Planned Treatment
The patient was simulated with the BodyFIX® (double-vacuum) immobilization system. The patient was positioned supine in a custom BodyFIX indexed vac-bag with arms above head. The patient was then levelled and straightened and a Vertical base line (VBL) (anterior and lateral markers) ascertained and marked on.
The vac-bag was then made and marks were placed on the bag with reference to VBL (which was later tattooed). The plastic thorax poncho was then placed on the patient and manifold and cushion positions were configured around VBL and located. The manifold was then attached to pump and poncho and vacuumed to maximum pressure -100 mbar. Three markers were placed over the vacuumed plastic sheet in line with the laser position and reference VBL – marks on vac-bag. Scans are zeroed at this level, and the plan isocenter position was referenced from this. There were no fiducial markers within the tumor or lung.
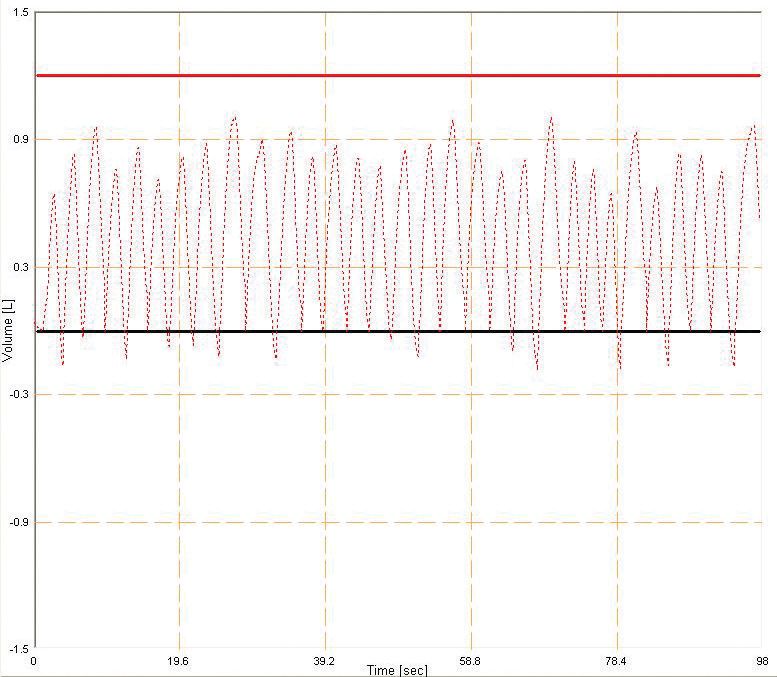
After immobilization was finalized, the Active Breathing Coordinator™ (ABC) system was used for monitoring and recording the patient’s breathing motion. The Active Breathing Coordinator, consisting of mouthpiece, tube and nose plugs was then attached to the pump and controller. Throughout the simulation process the patient’s breathing was monitored for consistency of breathing cycles and recorded for further comparisons. At this time, the patient was coached in breath-hold for inspiration and expiration scans, which also allowed the patient to become accustomed to the system. Once breathing was controlled the scan was started.
A Toshiba Aquilion™ large bore scanner was used but did not have the 4D option at the time of the patient simulation. A protocol was developed to account for breathing movement and three different scans were taken:
- Inspiration – patient holds breath on inhalation, ensuring movement is within normal breathing cycle amplitude and covering the entire lung, then reconstructed at 3 mm.
- Expiration – patient holds breath on exhalation, ensuring movement is within normal breathing cycle amplitude and covering the entire lung, then reconstructed at 3 mm.
- Slow acquisition / free breathing – 1 mm single slices with tube rotation speed decreased to the minimum are taken over the range of tumor position while patient breathes – usually 100 slices to allow adequate fusion accuracy.
The three scans were transferred to an Elekta Focal contouring station and the scans were named with the following convention:
Expiration = CT1exp (primary)
Inspiration = CT2insp (secondary)
Slow Aq. = CT3slowacq (secondary)
The expiration scan was used as the primary planning scan and the other two study sets were fused to it. The lungs, spinal cord, chest-wall and any other organs at risk (OAR) were contoured on the primary scan.
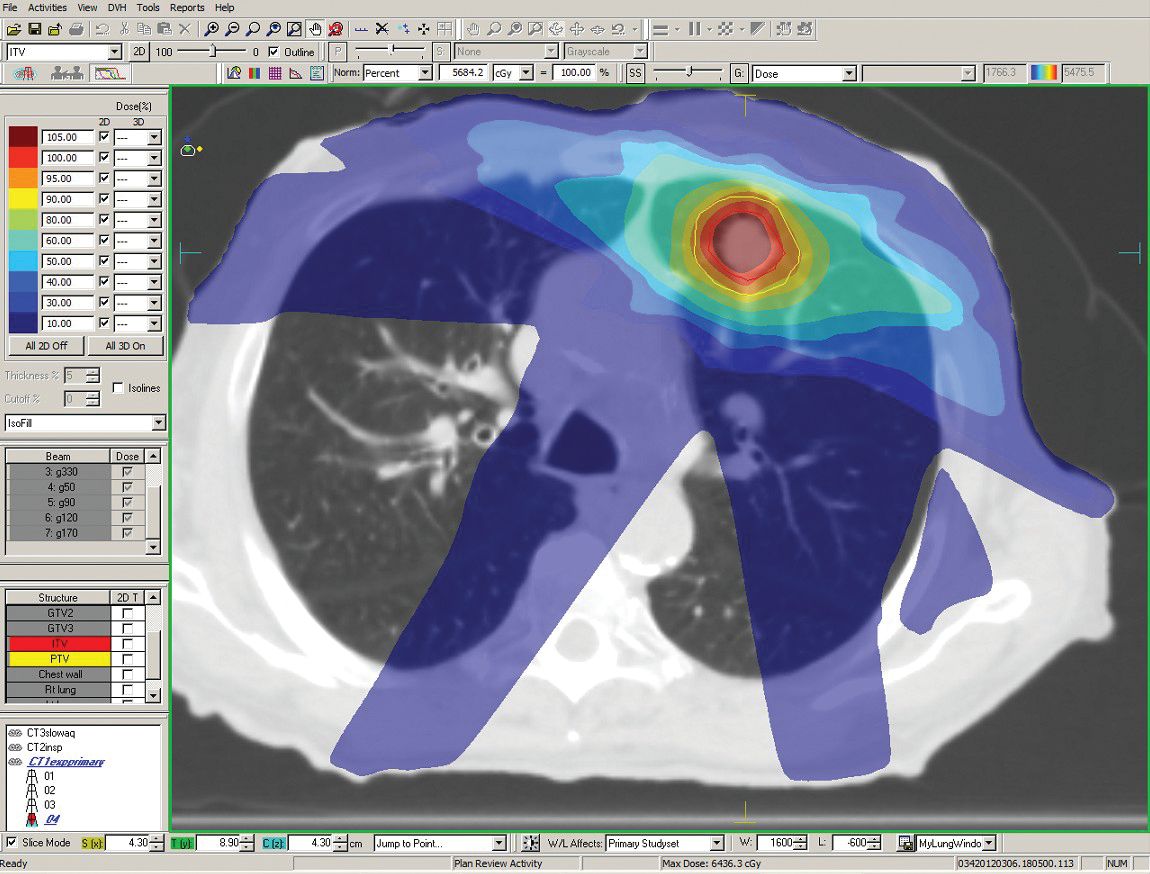
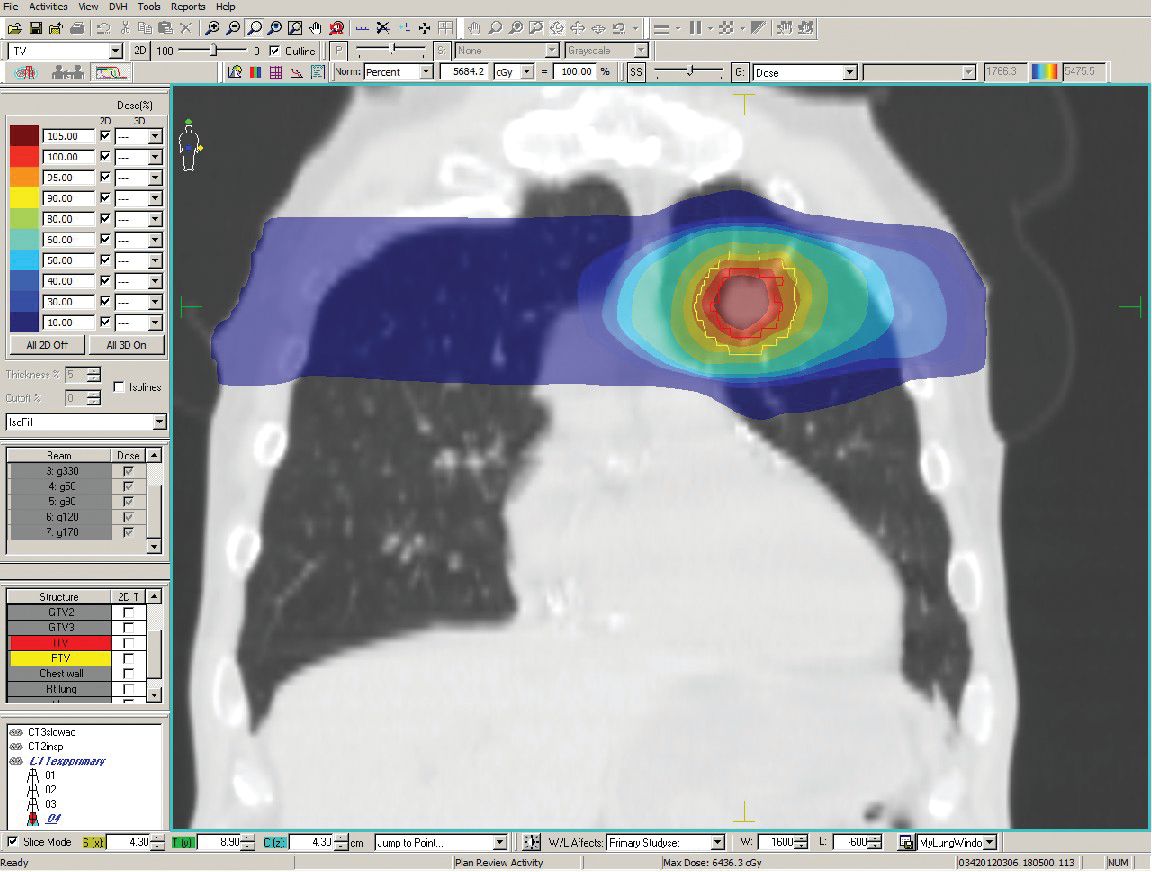
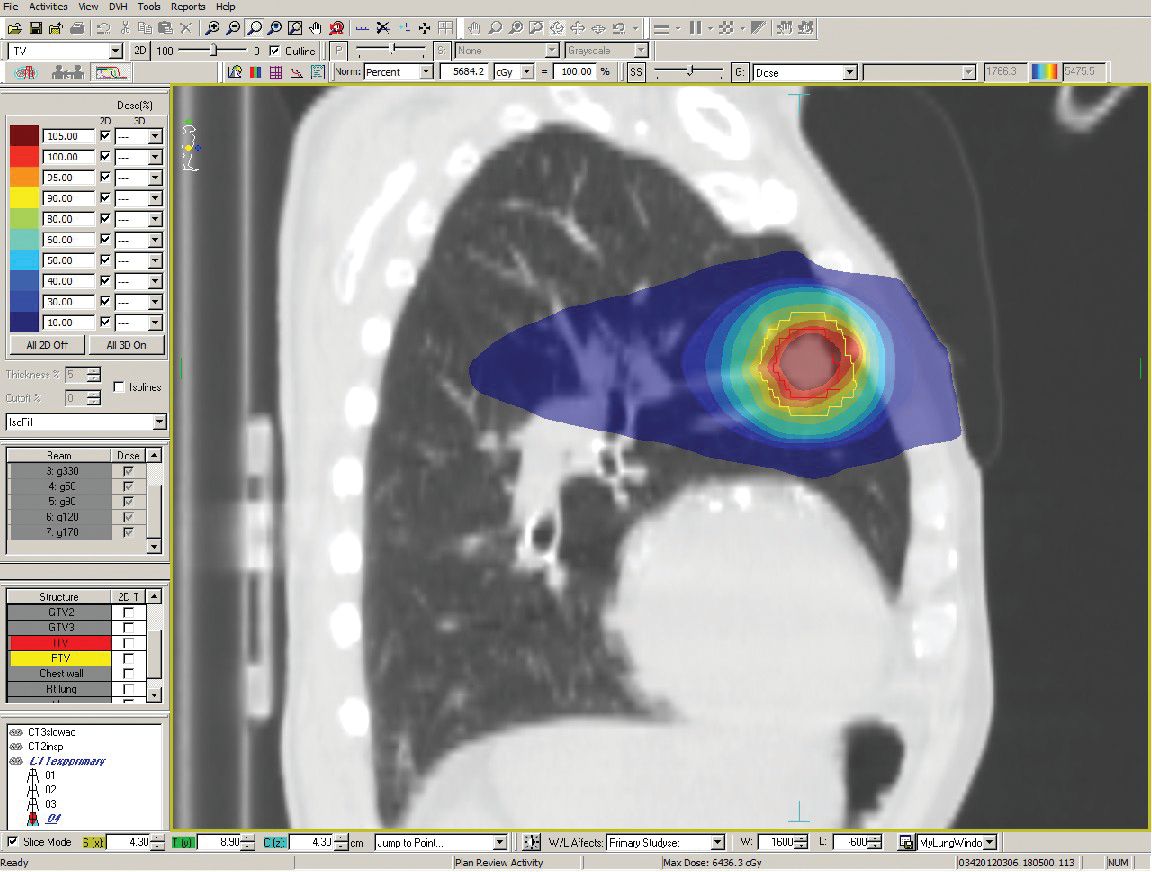
A GTV was contoured on each scan (using lung window level) and an ITV was created around all three contours (with no margin). The PTV was expanded by 6 mm around the ITV. This margin of 6 mm had been calculated according to Van Herk’s formula. [1]
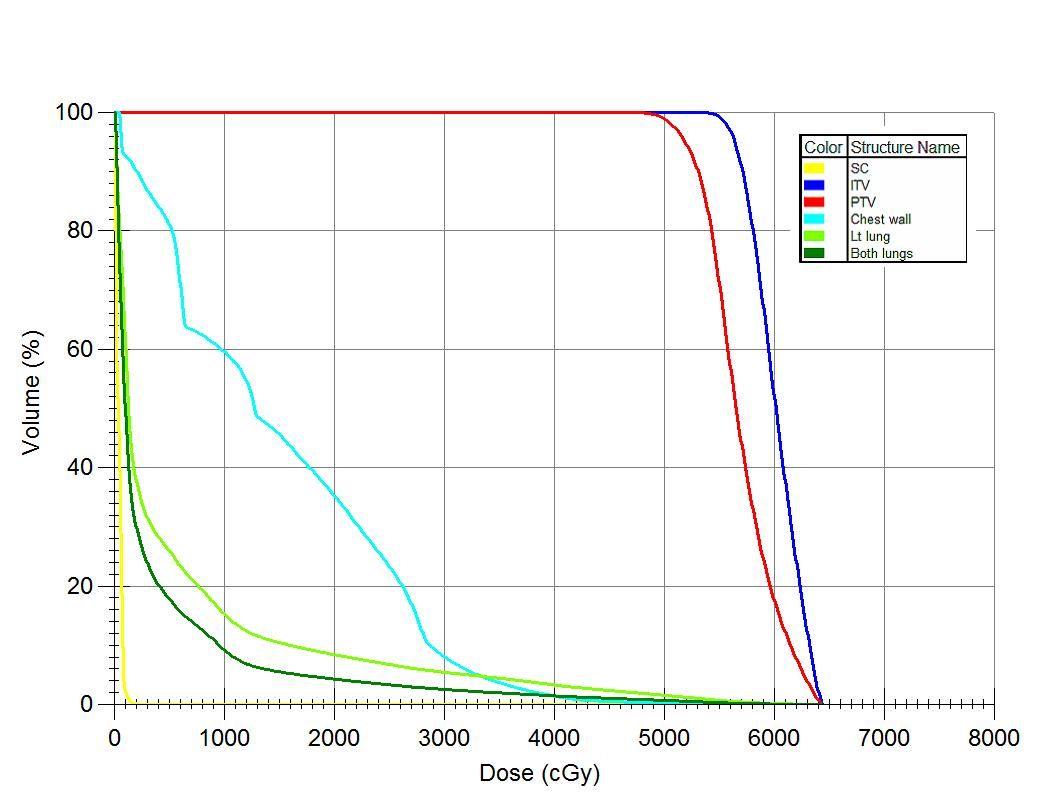
An Elekta XiO® V4.6 treatment planning system was used and a 10 MV 9 field fixed static beam 3D, conformal plan was generated with the isocenter at the center of the PTV. The specific structures to be avoided were the left and right lungs, spinal cord and the chestwall. The constraints were: both lungs V20< 10% (achieved: 4.3%); spinal cord <24 Gy (achieved: 3 Gy); chestwall V30< 30cc (achieved: 18 cc).
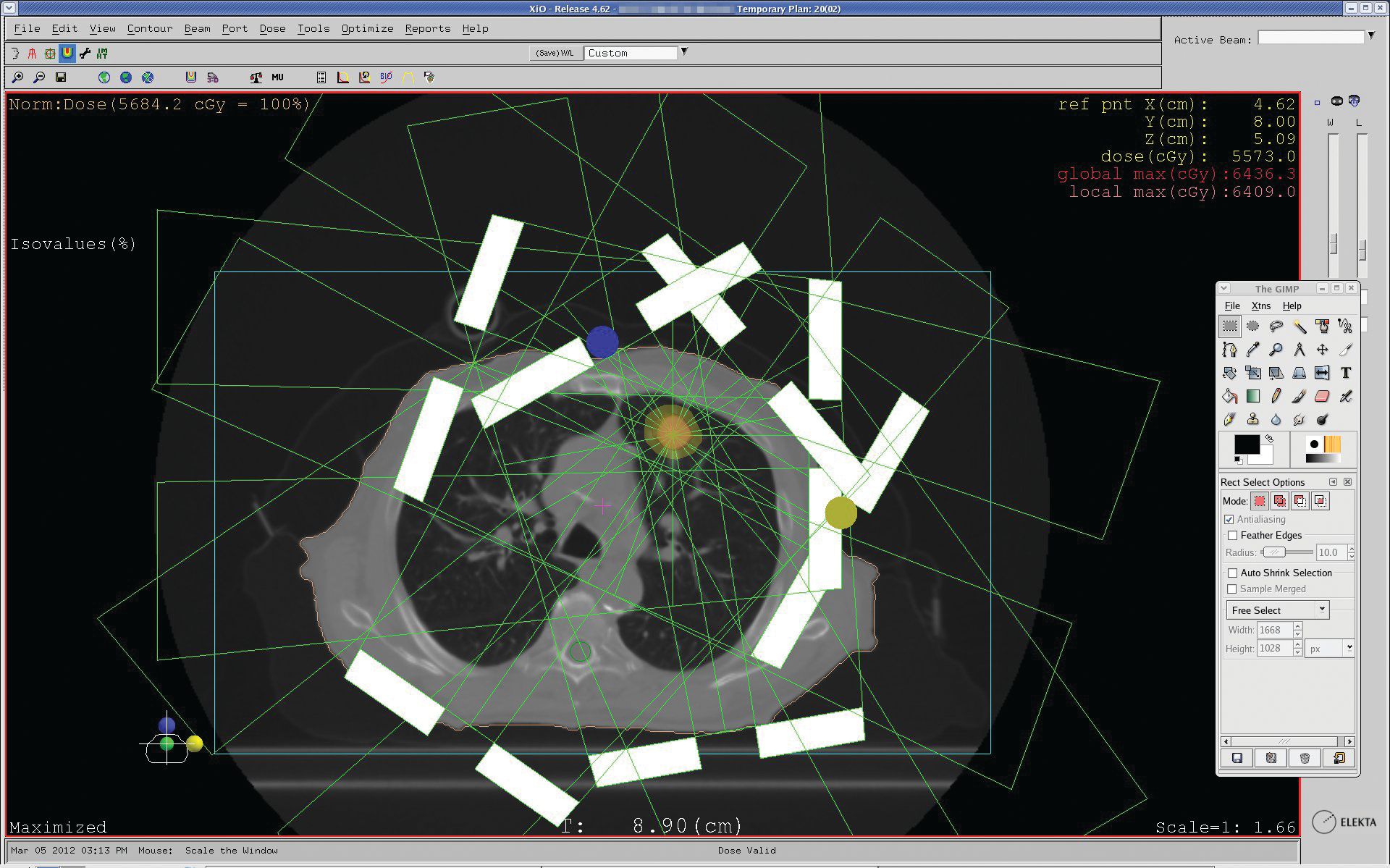
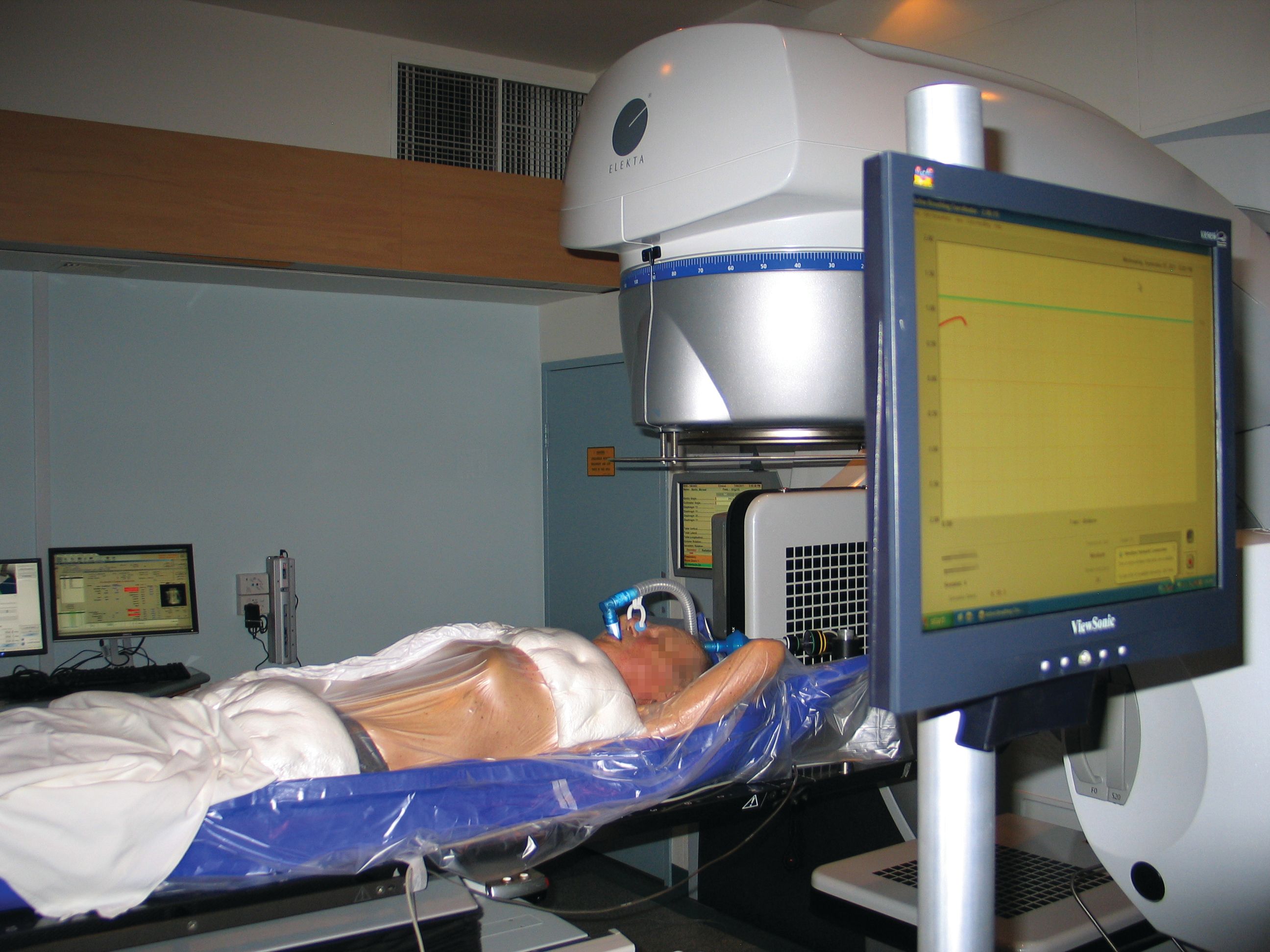
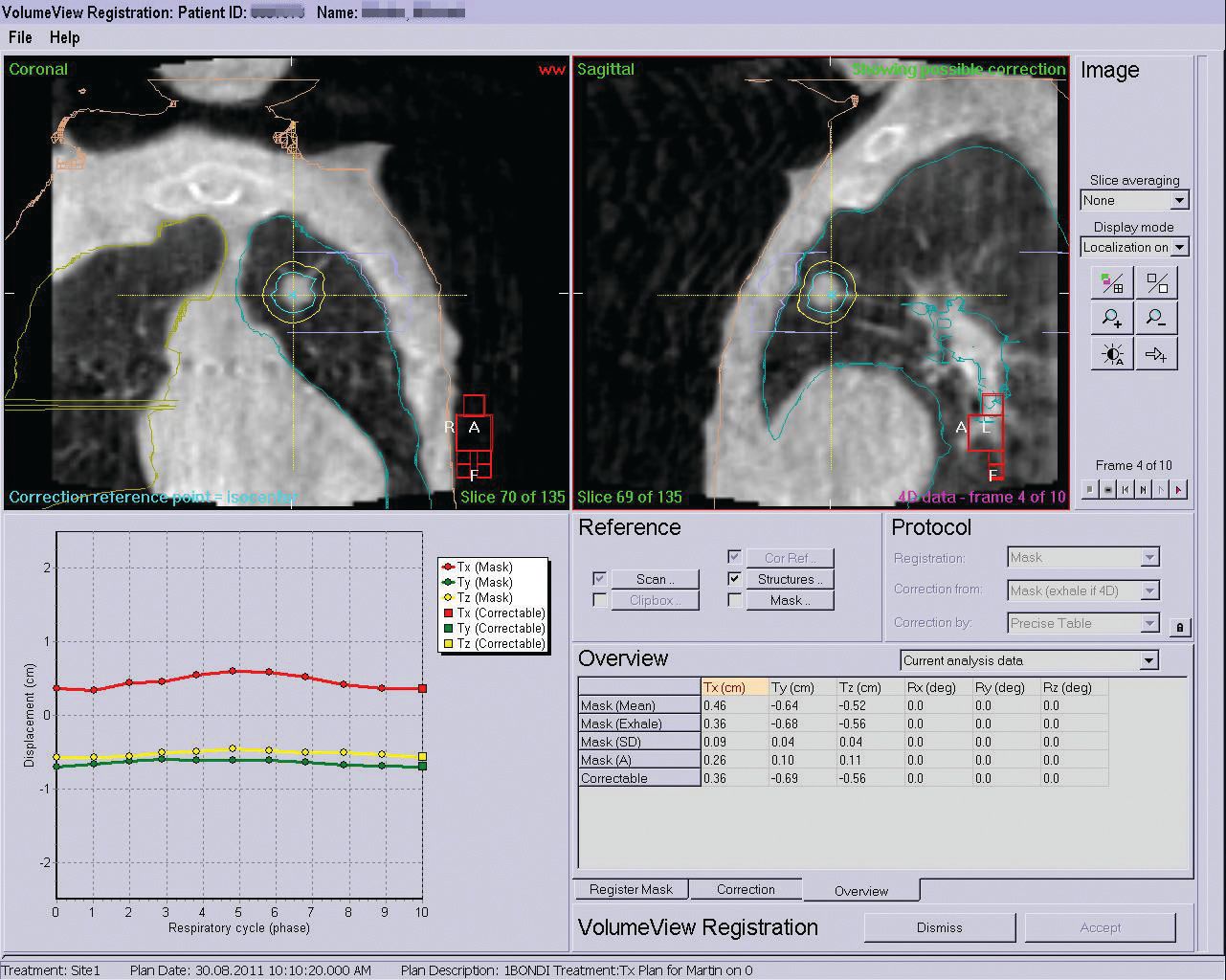
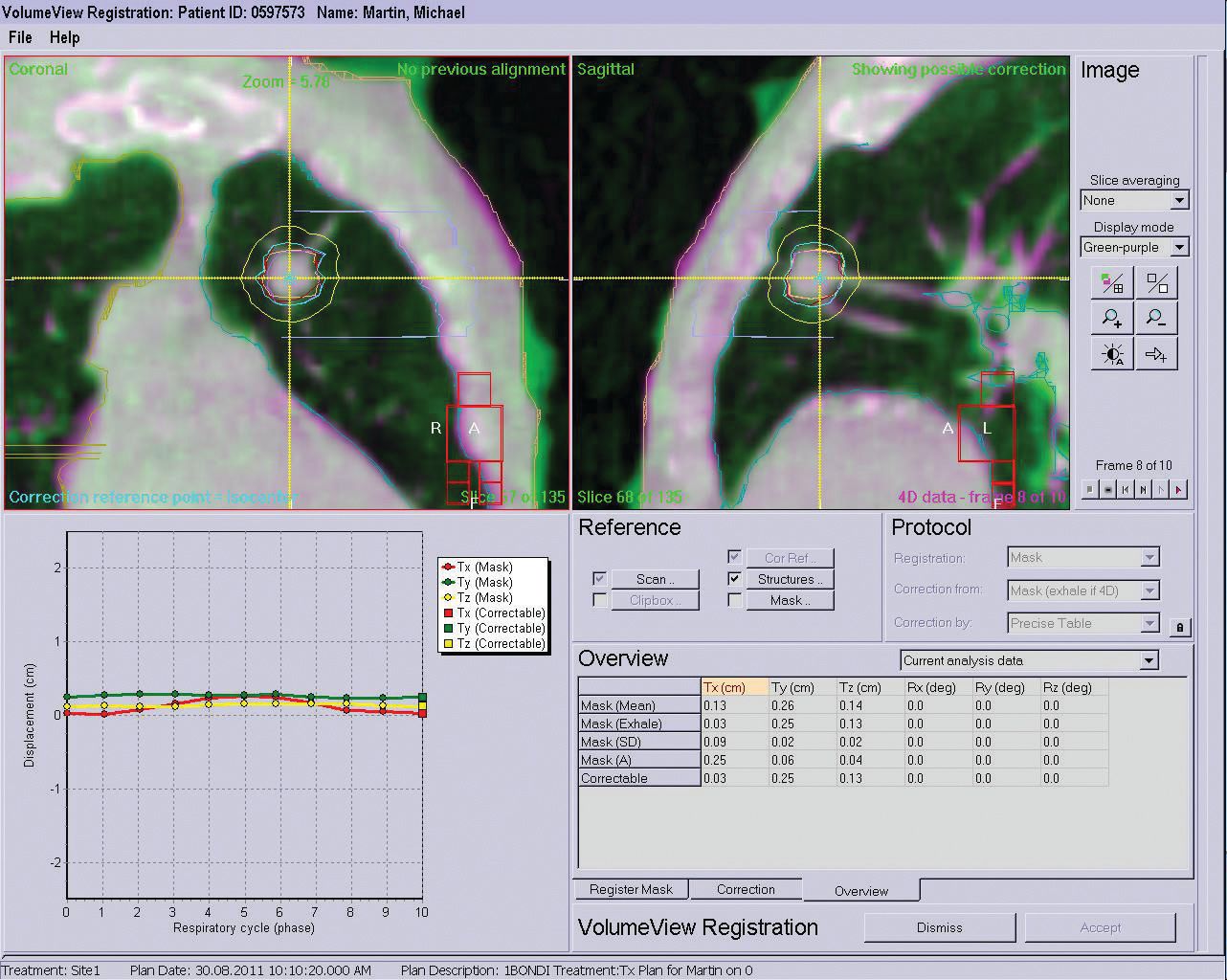
The patient was positioned on the treatment system in the same position for treatment as in the simulator /CT immobilization set–up. The Active Breathing Coordinator™ breath-monitoring equipment was setup once the plan isocenter position had been obtained and the patient’s breathing was monitored to attain regular breathing and the same amplitude as per the one obtained during the CT simulation process. Once the isocenter was confirmed and the outline checks (SSDs etc) were complete, a 4D Symmetry scan was performed with Elekta XVI 4.5 to allow exact positioning of the beams over the tumor movement. The slow acquisition bins projections by recognizing the movement of anatomy in the superior-inferior direction and reconstructs the Symmetry data sets for different phases of the breathing cycle allowing the exhale phase position of the tumor to be localized. The Symmetry CBCT scan was reviewed by the radiation oncologist at the treatment unit and fused with the planning (reference) exhale scan. Translation corrections were calculated based on mask registration on the maximum exhale phase and automatic movement shifts the couch. Another Symmetry scan was taken at completion of treatment to assess intra-fractionation movement. The duration of the treatment session and the imaging was 90 minutes and included the patient immobilization with BodyFIX® and Active Breathing Coordinator control. The nine conformational fields delivered 18 Gy per fraction in 20 minutes.
Outcome and Follow up
Six months after the completion of treatment the patient was well from the respiratory point of view. He denied any increase in shortness of breath or cough. He looked well on assessment.
A CT scan two months after treatment completion showed a decrease in the size of the left upper lobe lesion from 17 to 15 mm, no lung metastasis and no mediastinal or hilar lymphadenopathy.
Six months after the completion of treatment the chest CT showed 30% reduction in the size of the lesion. This case study was written seven months after treatment was completed and the patient remained well with no worsening of respiratory symptoms.
Discussion
This patient was the first patient treated with hypofractionated regimen for a primary lung tumor, with motion management provided by the 4D Symmetry CBCT online imaging and Active Breathing Coordinator™ monitoring. The treatment combined a number of Elekta products including Focal and XiO® planning systems, Active Breathing Coordinator, BodyFIX® immobilization, Elekta Axesse™ Linear Accelerator with Beam Modulator™ and 4D Symmetry CBCT imaging in XVI 4.5.
Due to the technology used, the radiation could be more directly focused on the tumor while minimizing the dose to surrounding lung, meaning a higher dose could be delivered confidently without increased toxicity. The treatment went smoothly and it was really impressive for a department without a 4D option available on the CT to see for the first time the movements of a real patient’s lung tumor provided by the 4D CBCT Symmetry scans. With the support of the Elekta team who were present for this Australian premiere, this first patient, who was also the perfect candidate for this experience, encouraged us to use the 4D Symmetry CBCT option of XVI 4.5 more often and with great confidence. The protocol developed will now apply to all patients suitable for curative hypo-fractionated SBRT at The Prince of Wales Hospital.
Reference
- The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy International Journal of Radiation Oncology*Biology*Physics, Volume 47, Issue 4, 1 July 2000, Pages 1121-1135, Marcel van Herk, Peter Remeijer, Coen Rasch, Joos V. Lebesque