RTTs assume key role in the adaptive radiotherapy workflow

How the radiation therapist's job description is expanding
In online adaptive radiotherapy, with images acquired, suitably trained radiation therapists (RTTs) perform online contouring to re-delineate targets and OAR to reflect the anatomical/functional changes of the patient at the time treatment1. For what has been traditionally a radiation oncologists’ role, RTTs are increasingly being called on to learn the skills necessary to recontour for daily adaptive re-planning, as departments gain confidence and optimize staffing requirements.
In FOCUS, RTTs Winnie Li and David Crawford reflect on their new and critical role in online ART as it is performed on their Elekta treatment systems.
Winnie Li, Radiation Therapy Manager, The Princess Margaret Cancer Centre
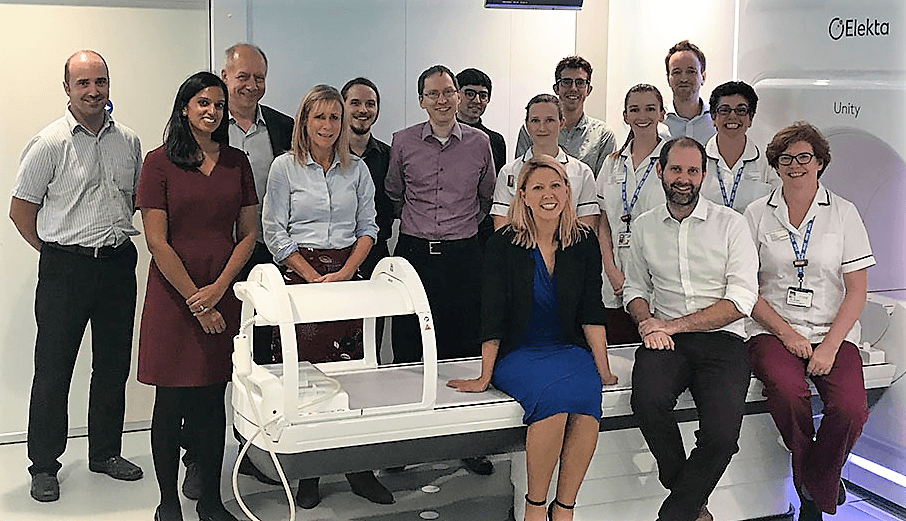
In 2019, when The Princess Margaret Cancer Centre (Toronto, Ontario) began using their latest Elekta system, Unity, the control room became a crowded place. A radiation oncologist, medical physicist and two RTTs presided over the treatment. The physician’s job was to recontour the OAR and target, and review the regenerated plan while physics assisted with plan review and QA.

“Over a year ago we established a program2 that enabled the therapists to develop the skills, knowledge and judgement to recontour online for both targets and OAR for whole gland prostate cancer patients from the second fraction onward,” says Winnie Li, MSc., MRT(T) Radiation Therapy Manager at Princess Margaret. “Essentially, we ushered the doctor and other personnel out of the room.”
Seven RTTs have received training for the online ART workflow and the center plans to train two more therapists. According to Li, the program will evolve by the end of 2023 to a therapist-led online ART workflow for oligometastases involving lymph nodes and bones.
Online ART processes
One aspect of the online adaptive workflow that unnerves some RTTs is the absence of room lasers to accurately set up and position patients, but this concern is quickly dispelled, according to Li.
“In reality, for an online ART workflow, as long as the patient is within the right range on the bed, it doesn’t really matter, because all translational and rotational displacements are accounted for during the replan process,” she explains. “You just adapt for it – you’re changing the shape of the target completely in every direction, so positioning is important, but not as imperative as on a regular linac.”
With the patient on the table, RTTs take a localization image to obtain the planning dataset and then initiate planning and contouring. Because this is the most time-intensive step, they acquire a verification MRI to ensure the target hasn’t moved too much prior to beam delivery.
“Online recontouring is especially important for the prostate, which is subject to shape change when rectal gas pushes on it.”
“For targets that move with respiration – such as abdominal oligometastases or liver or pancreas tumors – we will use cine MR to make sure targets are within a proper motion range,” Li says. “Online recontouring is especially important for the prostate, which is subject to shape change when rectal gas pushes on it. So, we’ve had cases in which we had to initiate a secondary adapt-to-shape plan adaptation.”
A striking example of the value of daily MR-guided ART was the case of a 65-year-old prostate cancer patient who immediately before MRgRT had a markedly enlarged pelvic mass involving the prostate with gross extra-capsular disease and invasion of the posterior bladder wall (Figure 1)3. The patient was referred for palliative radiation (36 Gy over six weekly fractions) to the pelvic mass to alleviate symptoms (i.e., urinary, pain, paresthesia).
“Unexpectedly, the target shrank 49 percent, and we were able to account for that in the online ART process,” she observes. “We generated a new reference plan after three fractions to add sacral plexus as an OAR, which wasn’t visible before due to mass encroachment.
“The unpredicted positive response of the target and improved symptoms showed us the value of the MR-Linac for online adaptive ART,” Li adds. “For every fraction we were able to recontour his target and spare his bowels and bladder.”

ART workflow requires multi-disciplinary collaboration
Because time is of the essence in the online adaptive workflow, the multi-disciplinary team (MDT) must work well together, with open channels of communication and clearly defined roles and responsibilities, Li says.
“At implementation, we mapped out the workflow in detail,” she recalls. “You don’t want overlapping responsibilities, because patients are only on the bed for a set amount of time – if you extend their time they start to move.”
The imperative to rapidly perform online ART to minimize the patient’s time on the bed had the team trying to accelerate processes at the start.
“When we started it was stressful in the room because every minute counted. Fortunately, the MDT had the right set of skills, knowledge and judgment to make it work.”
“In the beginning everyone was saying: ‘Can we go faster?,” Li remembers. “But the processes take what they take. You can’t contour faster, and you can’t contour half the target. When we started it was stressful in the room because every minute counted. Fortunately, the MDT had the right set of skills, knowledge and judgment to make it work.”
Bottom line is prudent resource allocation
As is typical in radiotherapy departments, there are far more RTTs than radiation oncologists, making it logical to shift more of the online ART tasks to the former group.
“If the contouring and recontouring skillset is transferable to a therapist and we’re there anyway, we should be taking on these tasks,” Li says. “In addition to contouring we educate and communicate with patients, and we understand their anatomy. That enables the doctors to spend more time assessing and consulting with patients.”
Li asserts that the online ART paradigm must shift to more body sites, which will entail rebuilding the program Princes Margaret developed for whole gland prostate to include oligometastases, pancreas, liver cases and other cancer types.
“During implementation it was difficult to get the oncologists’ time for a treatment session,” she says. “If we relied on the RO’s availability to plan and contour patients with online ART we would treat only four patients a day. For the program to grow and fill out the Elekta Unity schedule to its full potential, the workflow transitioned over to the therapist.”
David Crawford, RTT, GenesisCare St. Vincent’s Hospital
In Australia, training programs for radiation therapy are comprehensive, covering all the basics in addition to dosimetry and planning, making graduates well-suited to take on the entire radiotherapy workflow. For RTTs like David Crawford, this education would create an opportunity for him and two other GenesisCare St. Vincent’s RTTs to lead the Sydney center’s online adaptive workflow for prostate cancer patients.
“If the RTTs are a well-trained team it makes the RO’s job easier, and they can focus on the patient’s care plan.”
“Radiation oncologists bring in the patients and the radiation therapists carry on from there,” Crawford says. “If the RTTs are a well-trained team it makes the RO’s job easier, and they can focus on the patient’s care plan.”

In anticipation of expanding the RTT’s role in the online ART workflow following acquisition of a new Elekta treatment system in 2020, the center created a robust credentialing program modeled on a program at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research in London.
“We were able to contour several cases offline in a non-timed setting, then a number of cases online in the ‘pressure cooker’ setting of the patient on the treatment table, assessed by time and accuracy,” he says. “There’s no point in being accurate and slow, because the bladder is filling while it’s moving, and, similarly, there’s no point in being quick and inaccurate because that will cause a geographical miss.”
Teamwork is key to successful online ART
The much more time-sensitive nature of the online ART workflow versus the traditional offline process demands close collaboration among all members of the care team, Crawford stresses.
“It’s crucial,” he says. “There are so many different changes that can happen during treatment delivery that you need to think on your feet all the time and coordinate your actions with the radiation oncologist, the medical physics and nursing teams so that the patient journey is as smooth as possible.
“When you’re on an adaptive team, working closely is vital.”
“For example,” Crawford continues, “we do a lot of isotoxic treatments on Elekta Unity in which we have to go back and forth with the radiation oncologist, compromising on coverage in the hope that once we get them online we’re able to maximally boost up the target depending on where the organs-at-risk sit on that particular day. When you’re on an adaptive team, working closely is vital.”
Patient-related challenges also make the online ART workflow a race against time, according to Crawford.
“Patients might not have taken their Buscopan or anti-emetic medicine or followed their bowel prep or drunk enough water to fill their bladder,” he says. “We treat 12 to 15 patients back-to-back each day, so these patient issues can affect every other patient down the line. The entire team needs to be tightly-knit and think on its feet.”
The sim-less online ART workflow
For the last eight months, to improve the efficiency of the adaptive RT process for prostate patients, the St. Vincent’s team has been employing PSMA PET for planning in lieu of a CT or MRI scan for simulation. St. Vincent’s is the first in the world to implement PMSA PET in this sim-less workflow.

“The benefit of having a sim-less workflow is that we’re actually developing treatment plans on a diagnostic image,” Crawford says. “It benefits patients by having them avoid a couple of appointments in the department and it also reduces the resources we need and enhances department efficiency.
“The PMSA PET online workflow can only be done with Unity, because we know the system affords the ability to recontour and account for target shape changes,” he adds. “And we know there would be massive changes observed on a PMSA PET scan when prostate cancer patients haven’t had bladder or bowel prep.”
Redefining the RTT’s role
Arguably the inception of online ART has impacted the RTT more than any other professional on the care team, according to Crawford.
“Radiation therapists can be crucial in ensuring that online adaptive will evolve for the benefit of the patient.”
“Online ART is redefining our role within radiation therapy,” he says. “RTTs will definitely need to upskill themselves in adaptive techniques, as these techniques will continue to evolve. Radiation therapists can be crucial in ensuring that online adaptive will evolve for the benefit of the patient.
“It has really reenergized the staff,” Crawford adds. “Because radiation therapy is very process-driven, it can be monotonous at times. But with online ART, we have been given more meaningful responsibility, we’re learning new skills and techniques all the time. It has been a tremendously good thing for our profession.”
Learn more about Elekta’s radiation therapy solutions.
References
- Yen A, Shen C, Albuquerque K. The New Kid on the Block: Online Adaptive Radiotherapy in the Treatment of Gynecologic Cancers. Curr Oncol. 2023 Jan 8;30(1):865-874. doi: 10.3390/curroncol30010066. PMID: 36661715; PMCID: PMC9857810.
- Li W, Padayachee J, Navarro I, et al. Practice-based training strategy for therapist-driven prostate MR-Linac adaptive radiotherapy. Tech Innov Patient Support Radiat Oncol. 2023 May 13;27:100212. doi: 10.1016/j.tipsro.2023.100212. PMID: 37265510; PMCID: PMC10230256.
- Li W, Winter J, Padayachee J, et al. MR-guided adaptive radiotherapy, some room to maneuver. Front. Oncol., 14 April 2022, 12. doi: https://doi.org/10.3389/fonc.2022.877452.