Radiotherapy an indispensable modality at Teletón Children’s Oncology Hospital

Oncology center in Mexico boosts survival rate for children with cancer
The statistics on pediatric cancer in Mexico highlight a challenging problem, with the disease the second leading cause of death in children in the country, according to the 2010 Mexico census.1 Approximately 5,000 children are diagnosed with cancer each year, but many others go undiagnosed and many are diagnosed at late stages.2 According to Registry of Cancer in Children and Adolescents, the survival rate is 57.5 percent, which translates to a child dying of cancer every four hours.2
Teletón Children’s Oncology Hospital (HITO, Querétaro, Mexico) is among just a few hospitals in the world dedicated entirely to treating childhood cancers – including leukemia, lymphomas, central nervous system, bone and kidney tumors. The medical team approaches each case in a multidisciplinary manner, which allows the staff to arrive at a treatment plan and evaluate the patient’s response to treatment – a crucial factor in ensuring optimal lifelong care.
Imperatives and requirements for pediatric radiation therapy
When using radiotherapy to treat pediatric cancer, HITO staff prioritize accuracy due to the risk of significant long-term adverse effects that can compromise a patient’s quality of life.
“Precision is vital to achieving the appropriate dose to the tumor.”

“Precision is vital to achieving the appropriate dose to the tumor,” says pediatric radiation oncologist Beatriz García Robles, MD, deputy director of imaging, nuclear medicine and radiotherapy at HITO. “In children, we have to limit to the absolute minimum the dose to healthy tissues, thereby reducing the possibility of adverse effects. To that end, our Elekta Synergy® linac is equipped with the 160-leaf Agility MLC for highly conformal beam-shaping.”
HITO also operates a 64-slice CT system, an MRI unit and a PET CT machine, the images from which are fused for exceptionally precise contouring and treatment planning of targets and organs-at-risk (OARs). The most frequently used techniques for pediatric patients are 3D conformal radiation therapy and volumetric modulated arc therapy (VMAT), both of which afford a shorter treatment time than intensity modulated radiation therapy (IMRT).
For all of the center’s young patients, HITO runs a comprehensive support program that leverages technology to provide holistic care, focusing not only on the patient’s disease, but also offering psychological and social support to parents and siblings.
“For radiotherapy, we launched a psycho-behavioral program in which we explain the entire process with videos, cartoons, music and role-playing.”

“This program, which begins from the moment the patient and their family enter HITO, uses technology for diagnostic corroboration, active treatment, supportive care, surveillance and palliative care,” Dr. García Robles says. “For radiotherapy, we launched a psycho-behavioral program in which we explain the entire process with videos, cartoons, music and role-playing. As radiation therapy is a ‘puncture-free’ therapy, the patients are cooperative, which enables us to avoid the use of sedation for 80 percent of children under five-years-old.”
During the first few sessions, parents can observe the treatment through closed-circuit TV and even use a speaker to calm the patient and prevent him or her from movement by telling a story or by singing, she adds.
“Our integrated care management focuses on patient quality of life, stressing their physical, emotional and spiritual comfort,” she notes.
Over the last decade, the hospital has been steadily improving the outcomes for children with cancer.
“During 2023, we treated 890 patients, and the overall survival rate of patients treated in our hospital was 82.6 percent.”
“During 2023, we treated 890 patients, and the overall survival rate of patients treated in our hospital was 82.6 percent,” she notes. “Many of these patients received radiation therapy as a frontline or adjunctive treatment.”

The radiotherapy service opened its doors in February 2014, starting with a single morning session and with most treatments planned in 3D. Today, HITO’s radiation therapy department treats an average of 150 patients under 18-years-old each year. Radiotherapy techniques include VMAT, used in 65 percent of treatments and 3D conformal radiation therapy used for the other 35 percent.
While radiation therapy is a key modality at HITO, the tertiary center also has professionals in oncological surgery, medical oncology, nuclear medicine, neurology and neurosurgery, dentistry, cardiology, psychiatric oncology, pain clinic and palliative care. Advanced services include molecular and genetic diagnosis, in addition to a bone marrow transplant service that has performed 142 transplants since 2017, achieving a survival rate at Day 100 of 98 percent.
“Of these 142 patients, we used our Elekta Synergy linear accelerator to treat more than 60 percent with total body irradiation as part of the pre-transplant conditioning regimen [see Case 1] – a dose of 12 Gy for acute leukemias and 2 Gy as an immunosuppressive regimen for aplastic anemia,” Dr. García Robles says.
Anticipating even more advanced radiotherapy
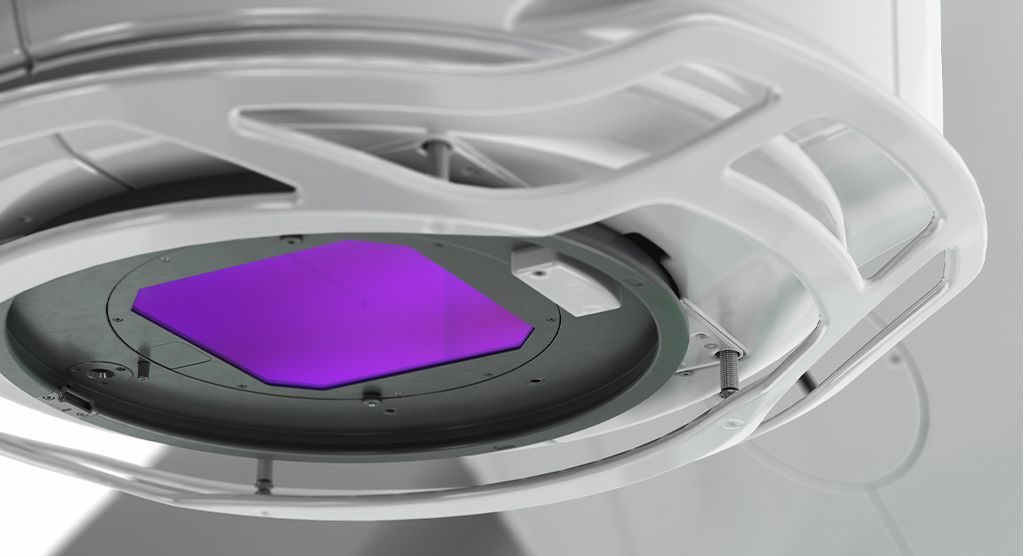
In 2025, Teletón Hospital will install the Elekta Unity MR-Linac and in 2028, HITO will acquire Elekta’s Versa HD™ linear accelerator.
“The integration of MRI with a sophisticated linac in Unity is a testament to our commitment to innovation.”
“The integration of MRI with a sophisticated linac in Elekta Unity is a testament to our commitment to innovation,” Dr. García Robles says. “The system will enable enhanced visualization and alignment of the primary tumor, for example, facilitating precise re-irradiation. This advanced technology will allow the use of smaller margins and daily adaptive planning, thus minimizing the dose to adjacent healthy structures.”
She adds that with Elekta Unity, staff will be able to significantly reduce the total number of treatment sessions – at least by a third compared to a conventional linac – without compromising results. This decrease in sessions will not only save time, but also minimize side effects in HITO’s patients, instilling a sense of hope and reassurance.
“Our patients can be assured that they will receive the best therapy based on their diagnosis, fully personalized to their response to treatment,” she says. “This commitment to precision medicine is a cornerstone of our care, ensuring that each patient receives the most effective and tailored plan.”
Case 1. A seven-year-old patient diagnosed with acute lymphoblastic leukemia in a pre-transplant conditioning protocol with total body irradiation.

As part of the pre-transplant conditioning, the patient received a total of 12 Gy in six fractions over three consecutive days, given twice a day with at least six hours between each administration. The treatment plan included contouring of all organs-at-risk to ensure that there were no hot spots. The 3D treatment plan involved two opposite fields prescribed source-to-surface distance to the iliac bone at a distance of four meters. The treatment was successful with favorable outcomes.
All plans made in the planning system (under Elekta authorization for planning at three meters), are verified with manual calculations and with in vivo dosimetry in the first session through optically stimulated luminescent dosimeters.
Case 2. A 15-year-old female patient was diagnosed with stage IIB Bulky Hodgkin lymphoma. After a partial response shown in PET2 (slow responder) she completed six cycles of ABVD chemotherapy and consolidative radiotherapy. The patient received 25.2 Gy in 14 fractions, targeting the initial sites of tumor activity, which included – as the CTV volume – the bilateral neck nodes, mediastinal nodes, and bilateral axillary lymph nodes.
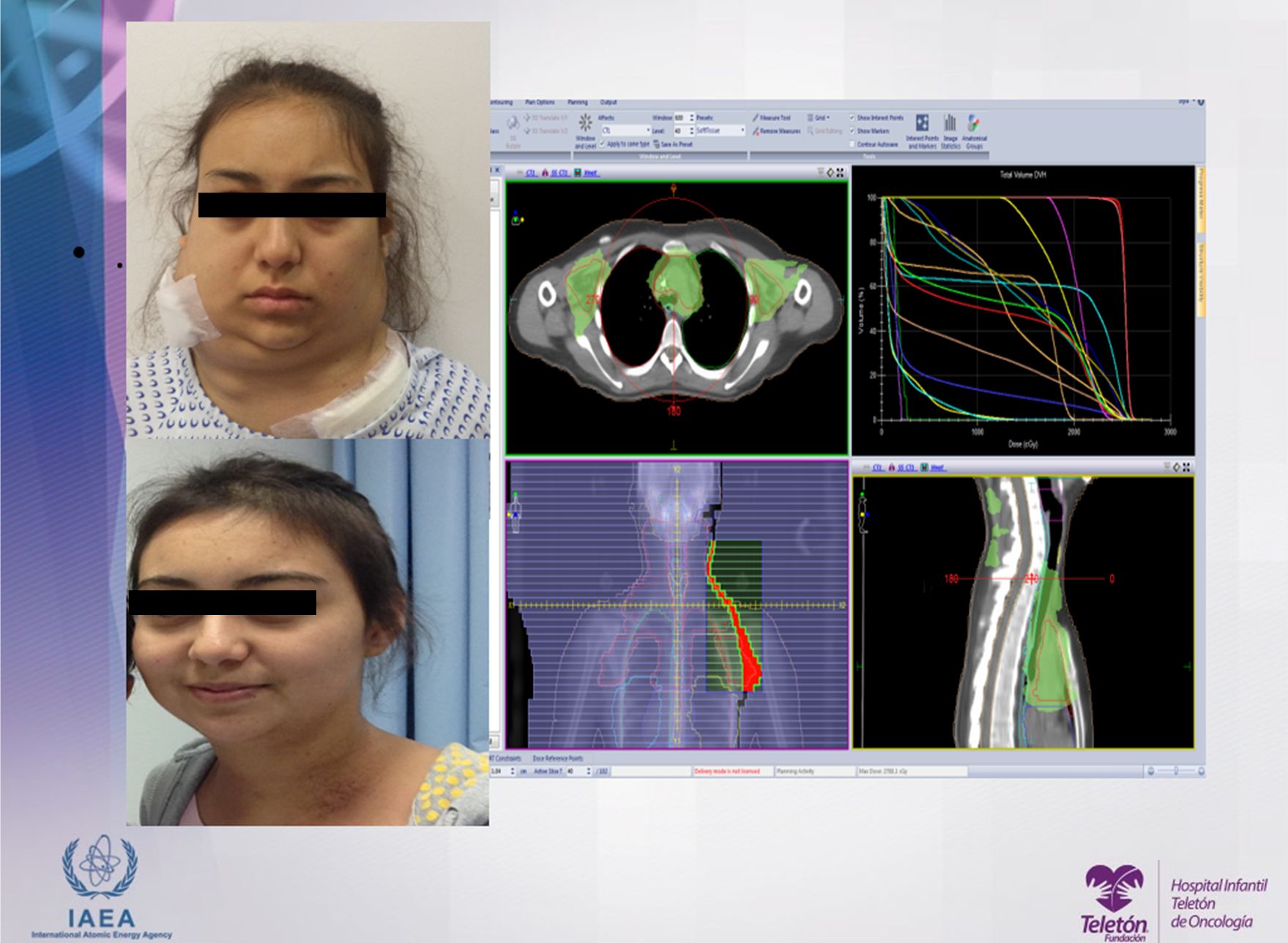
To account for potential differences in patient positioning, a 0.5 cm margin was added to the CTV to create the PTV. Clinicians used the VMAT planning technique to ensure that 95 percent of the prescribed dose covered the PTV while also maintaining the tolerance dose for the organs-at-risk.
The radiotherapy treatment was well tolerated by the patient, presenting only Grade 1 radiodermitis, which was treated with topical cream.
Learn more about radiation therapy with Elekta linacs.
References
- Censo Poblacional de la República Mexicana: Population Census of the Republic of Mexico, 2010. 2010, http://www.inegi.org.mx
- Rivera-Luna, R., Shalkow-Klincovstein, J., Velasco-Hidalgo, L. et al. Descriptive Epidemiology in Mexican children with cancer under an open national public health insurance program. BMC Cancer 14, 790 (2014). https://doi.org/10.1186/1471-2407-14-790
LAROX240815