Precision radiotherapy isn’t just for people
UK pet hospital uses radiotherapy to treat a spectrum of cancers in cats and dogs
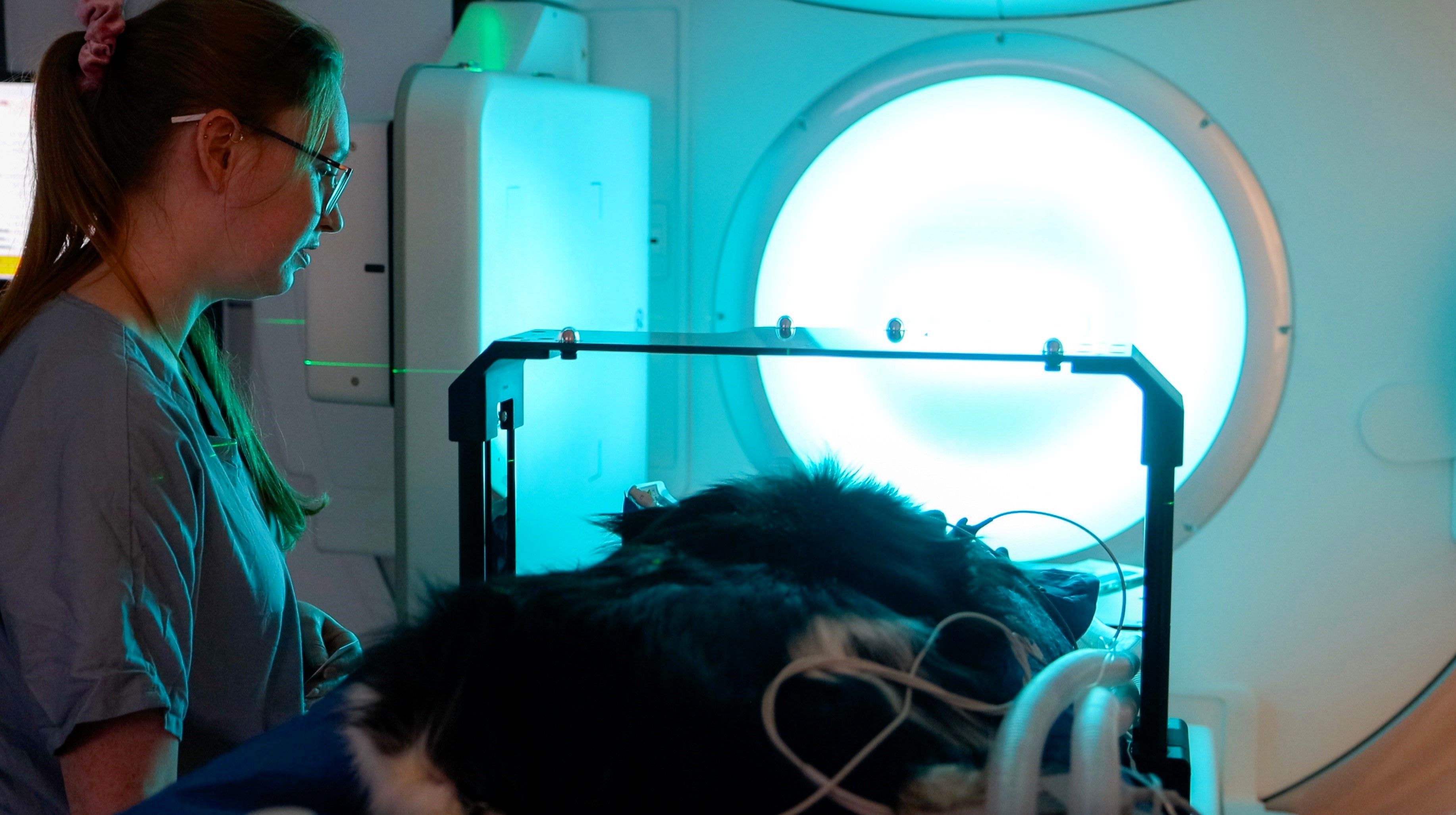
Just as people with cancer can benefit from radiotherapy, dogs and cats with cancer or other conditions, such as feline cystitis or osteoarthritis, can also benefit from the modality to cure or control cancer or to relieve pain. Since November 2023 – in a new 30,000 square foot facility – Bristol Vet Specialists (BVS, Bristol, UK) has been delivering radiotherapy to about 10 canine and/or feline patients each day. BVS is one of only seven veterinary care centers in the United Kingdom to offer its four-legged patients advanced radiation therapy and is the largest such medical center in the south of England and southwest Wales.

Reflecting the same level of compassion, care and sophistication as a human hospital, BVS offers afflicted pets the latest technology and treatments, including surgery, orthopedics, neurology and neurosurgery, internal medicine, ophthalmology, cardiology, dermatology, oncology and dentistry – as well as dedicated anesthesia, analgesia, diagnostic imaging and intensive care.
As BVS would be adding a radiotherapy service for the first time, the center’s Natasha Watts, RVN, BVS hospital manager, was tasked in 2022 to learn everything she could about radiotherapy and its application for dogs and cats and to use that knowledge to establish BVS’s radiotherapy department in the new facility (see sidebar).
Pet healthcare mecca
BVS opened in late October 2023, its total staff swelling in the coming months to about 140, approximately 40 of which represent the center’s many medical specialties. The oncology team consists of two medical oncologists, one Belgium-based radiation oncologist, a medical oncology resident, an oncology intern, three veterinary nurses and a radiation therapist (RTT).
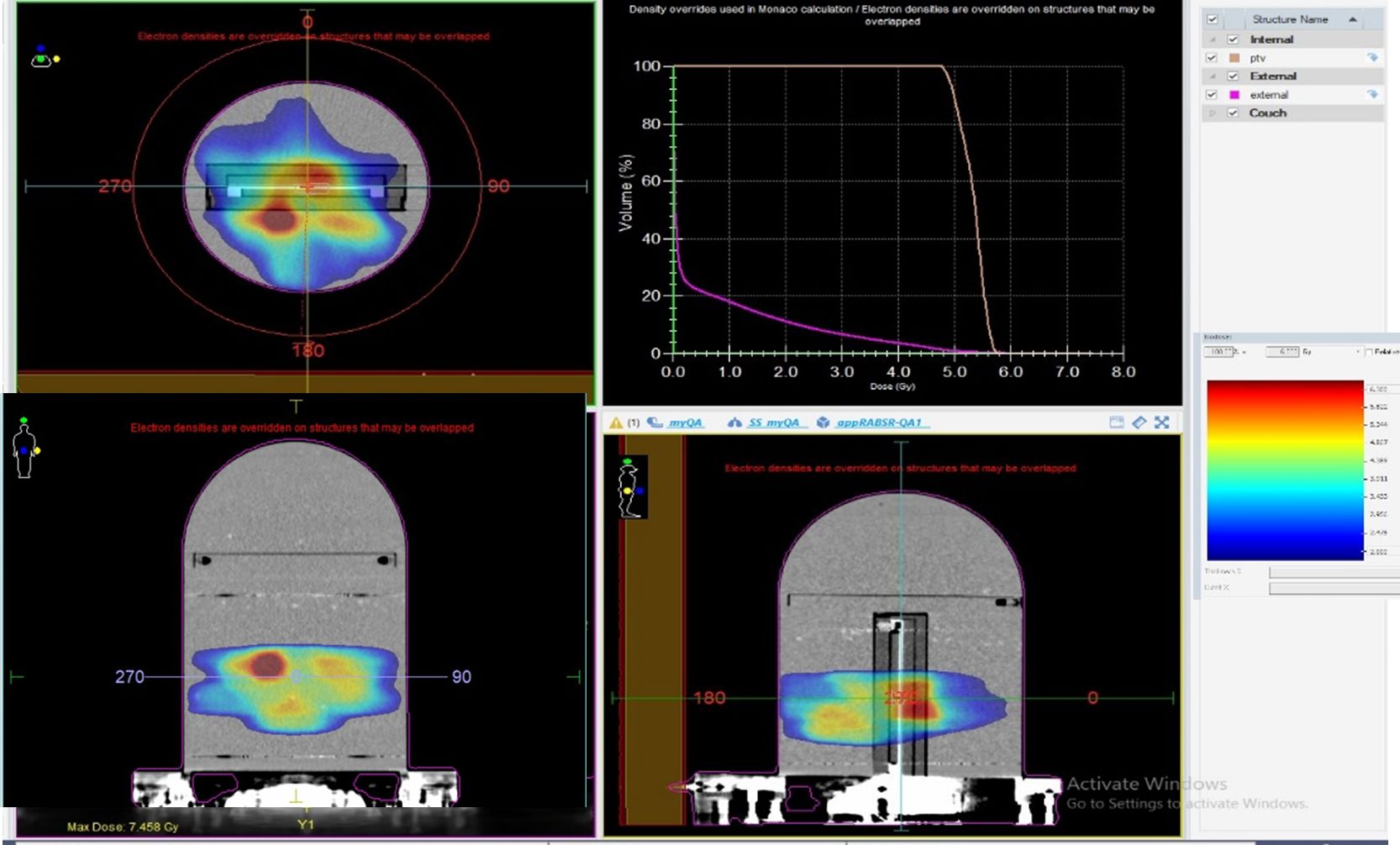
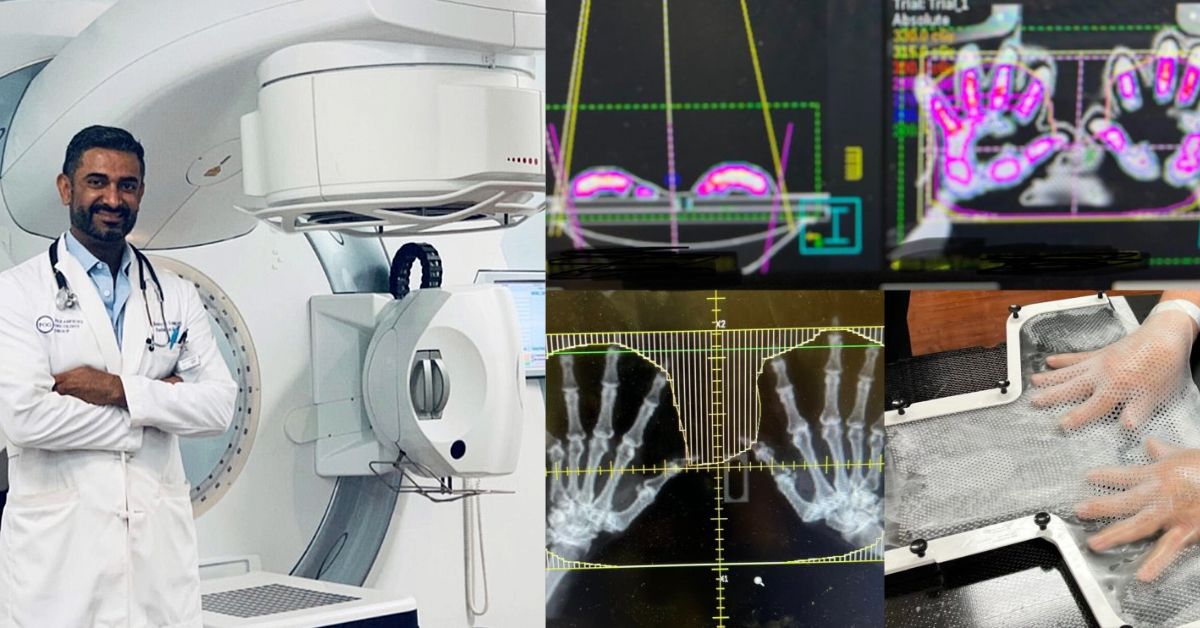
BVS’s radiotherapy technology includes an Elekta linear accelerator equipped with the Agility™ MLC for ultra-conformal beam shaping with Monaco® treatment planning and the HexaPOD™ evo robotic positioning system.

Beyond the linac’s technological sophistication, the center selected the system based on the support they knew Elekta and nearby Elekta users, Bristol Royal Infirmary, might provide, according to Dr. Owen Davies, head of the BVS oncology department.
“Bristol Royal Infirmary is a large human hospital with five Elekta treatment machines, so we knew we could count on their physics and planning software support,” says Dr. Davies, an American and European RCVS oncology specialist. “Moreover, we appreciated that Elekta equipment service would be close by. For example, we had a recent issue with the MLC and an Elekta field service engineer came over very quickly and fixed it.”
Radiotherapy a mainstay at Bristol Vet Specialists
While many BVS cases involving the most virulent cancers entail multi-modality treatments – surgery, radiotherapy and chemotherapy – half of the center’s workload is radiotherapy-only.
“Eighty percent of the radiation therapy is VMAT – 75 to 80 percent of which is done with curative intent – and nine percent is hypofractionated.”
“Eighty percent of the radiation therapy is VMAT – 75 to 80 percent of which is done with curative intent – and nine percent is hypofractionated,” Dr. Davies notes.

Potent doses are used in VMAT for pets due to their shorter life spans compared to people, he says.
“In general, we worry less about the potency of IMRT for animals than for humans, the idea being that you would expose a wider volume of the body to non-therapeutic beams, but still need a radiation dose,” Dr. Davies explains. “Our patients don’t live as long, so they have less time to pick up subsequent mutations in their genome that can result in cancers. Therefore, if the natural survival of a dog might be three- or four more-years post-treatment, then the use of IMRT isn’t such a big issue.
“Hypofractionated radiotherapy is very useful for palliative cases,” he adds. “That will involve lower doses and fewer sessions. We also consider hypofractionation to control pain in cases of unresectable tumors, or for very radiosensitive tumors such as lymphoma or myeloma.”
Typical dog and cat radiotherapy indications
Pets present with a spectrum of different cancers, including partially resected solid tumors, such as carcinomas and sarcomas, oral tumors – either in the gross disease setting or after incomplete resection – some types of lymphomas, and many different mast cell tumors.
“Mast cell tumors don’t have a good similarity in humans, which in people is a type of leukemia, whereas in dogs, for example, they can be very radiosensitive,” Dr. Davies says.

Whether the animal is young or old, the majority of animal cancers are diagnosed at advanced stages, due to the inherent stoicism of dogs and cats.
“You and I might go to the doctor if we’re feeling a little breathless climbing stairs,” he says. “It’s hard to appreciate things like that in a dog or cat until the disease advances to a point at which they don’t go up the stairs at all. These animals try to hide signs of disease – they try to make good and get on with their life.”
Older cats and dogs are more prone to developing cancer, but – just as in people – cancer doesn’t respect age.
“We have treated dogs as young as two-years-old,” Dr. Davies says. “At the moment, we are treating a four-month-old dog with a nephroblastoma, for which he has had surgery to debulk the tumor and is presently receiving adjunctive radiation to treat the tumor roots.”

Treatment preparation and procedure
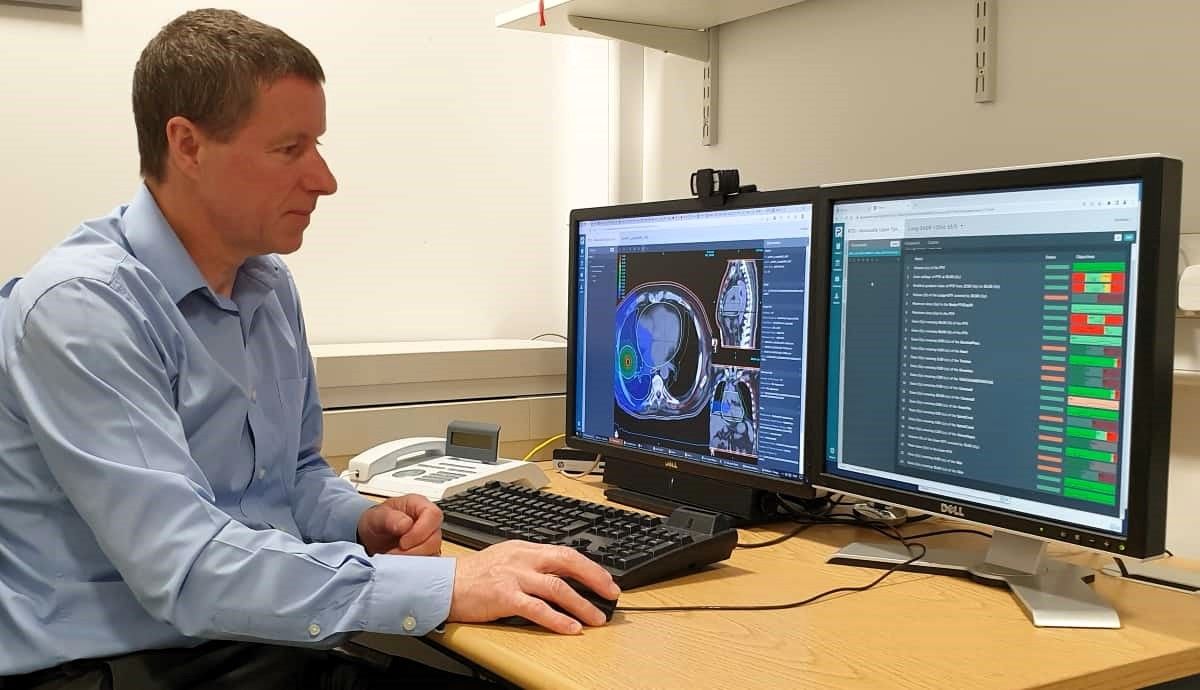
The key to prepping cats and dogs for radiation therapy is secure immobilization, which requires the judicious use of vacuum bags for most patients. For head tumors and other cranial pathology, BVS uses dental putty on a Perspex bridge and a thermoplastic mask. All cats and dogs are anesthetized during treatment. Treatment planning is done remotely.
“The main difference between planning for human radiotherapy and planning for animals is the dose level to organs-at-risk,” he says. “We might accept higher doses because our patients have a shorter post-treatment natural life expectancy. In general, we would be doing more palliative treatments for pain control and inflammation reduction purposes rather than tumor treating purposes.”
Grateful owners
The guardians of the feline and canine patients who have been treated at BVS since late 2023 – whether it be with surgery, chemotherapy or radiotherapy – have expressed gratitude for the center’s care of their pets.
“It has taken the profession a long time to realize that you don’t have to make dogs or cats ill with cancer treatments to achieve an acceptable outcome.”
“Pet owners are thankful because vets, in general, are somewhat nervous about treating cancers,” Dr. Davies observes. “It has taken the profession a long time to realize that you don’t have to make dogs or cats ill with cancer treatments to achieve an acceptable outcome. The reason why humans can sometimes become ill is because they might have another 40 or 50 years to fight for. An animal wouldn’t have that, so it would be foolish to try and treat them with such an intense and aggressive therapy.
“Consequently, many vets still assume that cats and dogs will get dreadfully ill throughout treatment,” he adds. “That’s really not the case. There are many people who come to us having been made to feel guilty by their local vet practice for even suggesting their animal should have treatment and not be euthanized. So, generally, owners view oncology services favorably, because we’re the vets who listen and care about them and will accompany them in their pet’s cancer treatment journey.”
Veterinary nurse spearheads establishment of BVS radiotherapy service
BVS, formerly known as Highcroft Referrals (Bristol, UK) – where it shared a building with Highcroft Veterinary Hospital until October 2023 – would add a radiation therapy service in the new, multidisciplinary veterinary hospital.
With no radiation therapy experts on staff at Highcroft Veterinary Hospital or BVS (still physically located at Highcroft at that time), the latter needed to tap someone – regardless of the individual’s radiotherapy experience – to make its radiation therapy department a reality. The hospital recruited BVS’s Hospital Manager Natasha Watts, RVN to jump into the breach.
“Since I was the hospital manager, and because I had a nursing degree, they determined that I would be the person to lead the radiotherapy project and get it off the ground.”

“Since I was the hospital manager, and because I had a nursing degree, they determined that I would be the person to lead the radiotherapy project and get it off the ground,” Watts recalls. “I had to go from knowing zero about radiation therapy to understanding at least a little bit more at this moment in time. It was a steep learning curve.”
BVS contacted Bristol Royal Infirmary, a center with five linacs, and asked them to educate Watts on what she needed to know. She began joining monthly meetings at the hospital in November 2022, accelerating the pace to weekly meetings from December 2022 onward as construction on the new site continued.
“I met with the physicists there and they were brilliant,” Watts recalls. “They explained a lot about radiotherapy and linacs, the procedures, and how things worked, such as positioning and immobilization equipment like vac bags and thermoplastics. We tried to get all these things ordered way before we needed them, and we got the team from the thermoplastics company to teach Bristol Royal Infirmary therapeutic radiographers (RTTs) – who would rotate through BVS – how to use them on animals. That was also a learning curve for that company since they don’t make thermoplastics for use on animals, which are quite hairy – so there was a little bit of waxing going on.”
Royal Infirmary RTTs would work at the veterinary hospital on a year’s contract; two RTTs would work at BVS for month then return to the Royal Infirmary and replaced with two other RTTs.
“I think working with animals is interesting for them if they are so inclined,” she observes. “It’s a huge learning curve, regardless, to master things like positioning to get dogs and cats into these weird and wonderful angles compared to what they would do with a human.”
Watts adds that the RTTs who rotate through BVS diligently take notes on what works positioning-wise and what tweaks need to be made, and then make these notes available to the incoming replacement RTTs.
“In theory, positioning shouldn’t be an issue because the animals are asleep,” she says, “but we put breathing tubes down and that makes it trickier to orient the positioning equipment. The RTTs’ notes on how to do these things were invaluable to the next RTTs coming in.”
Learn more about veterinary radiation therapy with Elekta solutions.
References
- Roberts E, Shirlow A, Cox A, Davies O. Multiple myeloma involving the gastrointestinal tract in an English Springer Spaniel. Vet Med Sci. 2022 Nov;8(6):2273-2276.
- Davies O, Taylor AJ. Refining the “double two-thirds” rule: Genotype-based breed grouping and clinical presentation help predict the diagnosis of canine splenic mass lesions in 288 dogs. Vet Comp Oncol. 2020;1–11.
- Purzycka K, Peters LM, Desmas I, Davies O, Chang Y-M, Lara-Garcia A. Clinicopathological characteristics and prognostic factors for canine multicentric non-indolent T-cell lymphoma: 107 cases. Vet Comp Oncol. 2020;1–8.
- Davies O, Szladovits B, Polton G, Garden OA, Leo C, Lara-Garcia A. Prognostic significance of clinical presentation, induction and rescue treatment in 42 cases of canine centroblastic diffuse large B-cell multicentric lymphoma in the United Kingdom. Vet Comp Oncol. 2018;16:276–287.
- Davies O, Spencer S, Necova S, et al. Intranasal melanoma treated with radiation therapy in three dogs. Veterinary Quarterly (2017), 37:1, 274-281.
LAROX241121