Optimizing teams and resources with the provision of brachytherapy in one room
Dr. Umesh Mahantshetty reflects on how using a single room for placement, imaging and treatment benefits patients
Brachytherapy needs a combination of the right technology and well-trained staff to deliver optimum results for every patient. But for many hospitals, this means moving patients between departments.

“If I was the patient, and I’d been told that each part of the treatment was happening in a different room, I’d feel anxious and confused,” says Dr. Umesh Mahantshetty, Radiation Oncologist at Homi Bhabha Cancer Hospital & Research Centre in Visakhapatnam (a unit of Mumbai’s Tata Memorial Centre). “And I’d be worried as to how much pain or discomfort I’d undergo as I’m being wheeled around.”
Keeping a patient in one room for placement, imaging, and treatment helps them feel much more at ease. “It not only reduces stress on the patient, but also on clinicians and hospital resources,” says Dr. Mahantshetty.
The challenges of multi-room treatment
Two decades ago, the Tata Memorial Centre installed its first integrated brachytherapy unit. “At that time, 2D imaging and the High Dose Rate (HDR) unit were in the same room as the operating table,” explains Dr Mahantshetty. “But as technology advanced, this one-room solution took a back seat due to use of fluoroscopy, and people had to be taken elsewhere for imaging.”
Their workflow at this time followed four distinct phases:
- Placement of the applicator, often done in a minor operating theater in OT Complex.
- Wheeling the patient to Radiology/Radiotherapy Department for imaging, accompanied by a nurse.
- ‘Parking’ the patient for 1 – 2 hours or so while images were assessed, and the treatment planned.
- Taking the patient to a fourth room (Treatment Unit) for treatment.
“There are a lot of uncertainties in a journey that involves up to four different locations and several different staff members,” explains Dr. Mahantshetty. “It becomes a nightmare to train everyone involved in all these processes. The movement makes it harder to keep the applicators in the right place and the patients in the right position. And there’s only one chance to get a good image set for planning.”
The team also needed to find a suitable space for patients to recover from anesthesia, and staff available to monitor them. And if there were any issues, the treating physician had to be informed and the team made ready to solve the problem.
“We can all see what’s happening in real-time and this means we can give the patient the best treatment as efficiently as possible.”
Three reasons to keep brachytherapy in one room
Since the team has moved to a single-room brachytherapy solution, they’ve experienced significant benefits:
- Optimized workflows: A busy brachytherapy environment becomes a lot easier to manage when everyone’s in one place. “We can all see what’s happening in real-time,” says Dr. Mahantshetty. “And this means we can give the patient the best treatment as efficiently as possible. If there’s any kind of query, the team is already there, and immediately ready for whatever has to be done.”
- Maximized resources: A single-room solution uses fewer hospital resources. It eliminates staff downtime as they move patients between departments and frees up rooms for new opportunities.
“We can perform accurate placement in a shorter time by giving clinicians access to fast in-room 2D and 3D imaging,” says Dr. Mahantshetty. “And there’s a reduced chance of implant movement because the patient is not being transported. This streamlines the whole process, saving time and enabling us to see more patients without compromising on the quality of their treatment.”
- Better outcomes: Advances in image-guided adaptive brachytherapy mean that tumors and organs at risk can be accurately identified. “We feel confident to deliver very high doses of radiation to the target area while at the same time protecting the surrounding tissue,” explains Dr. Mahantshetty. “It leads to excellent outcomes in terms of tumor control rates, as well as acceptable toxicities.”
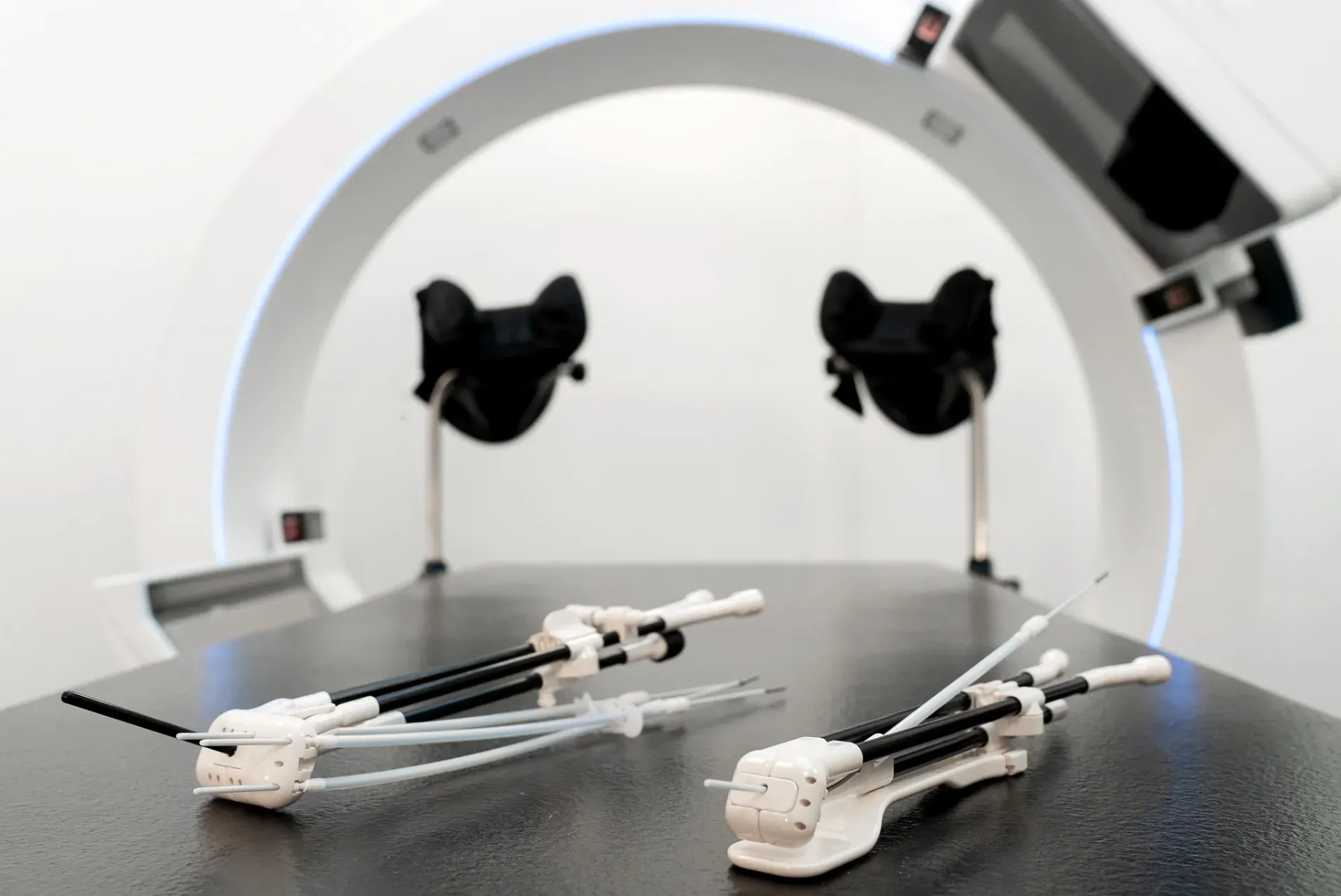
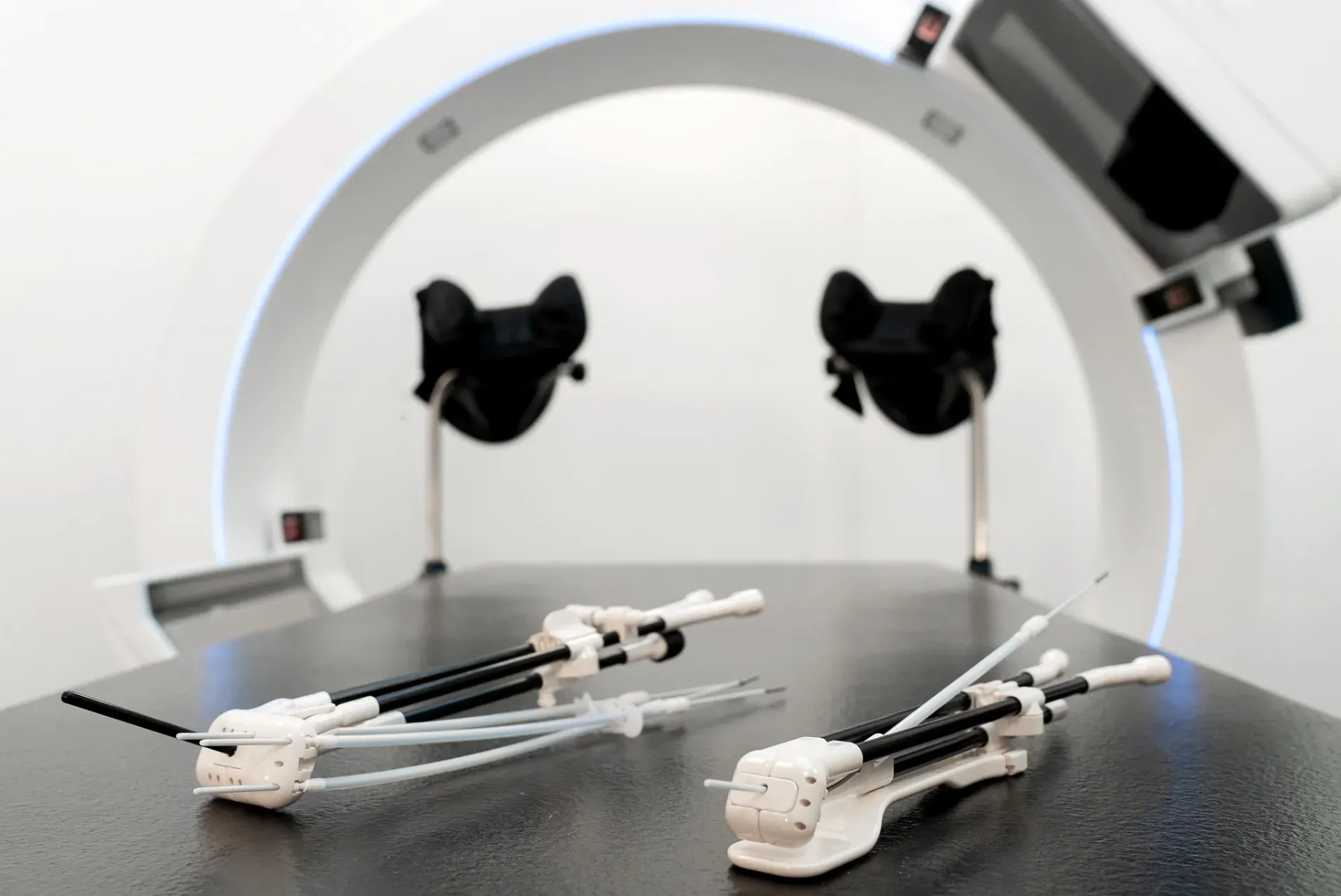
Maximizing efficiency with two rooms
Of course, one room may just be the start. “When I look at logistics across the many busy cancer centers in the world, I think the ideal would be two brachytherapy rooms set up side-by-side for two different patients,” says Dr. Mahantshetty.
“Once you finish the applicator or needle placement and imaging for the first patient, you can go to the next room and do the implantation and imaging for your second patient. While that’s happening, the treatment planning for the first patient is performed. After you’ve finished imaging the second patient, the first patient’s treatment is started. Then you do the same steps for the second patient while the first room is made ready for a third person.”
By working from two well-equipped rooms like this, busy hospitals could significantly increase their efficiency and maximize the number of brachytherapy patients they can see.
The importance of image-guided brachytherapy
Cervical cancer outcomes have improved in the last 15-20 years because of the advances in brachytherapy. “With the implementation of image-guided adaptive brachytherapy, the outcomes today are something which people only dreamt of 15 or 20 years ago,” says Dr. Mahantshetty. “We have tumor control rates of 90% above the irrespective stage of locally advanced cervical cancer.”
“With the implementation of image-guided adaptive brachytherapy, the outcomes today are something which people only dreamt of 15 or 20 years ago.”
This is partly due to improvements in the applicators that are available to patients today. But a lot of it is also due to 3D imaging, which enables teams to check the progress of tumors after external radiation beam therapy, as well as accurately identify organs at risk. It puts teams in a much better position for accurate treatment planning. And with ongoing research and the rapid evolution of technology, improvements in brachytherapy are set to continue.
Getting the best from technology
While technology is incredibly valuable, it’s only as good as the people who are operating it.
“A lack of skills is one of the major hurdles for brachytherapy today,” says Dr. Mahantshetty. “Which is why it’s so important to train practitioners, through hands-on workshops and regular training.”
He has already started working on a brachytherapy research center, supported by Elekta, to encourage wider use of brachytherapy worldwide. Through the BrachyAcademy, he’s developing modules that can be perfected and pushed into the community for training.
“My dream is that the skills of brachytherapy will be imparted to all trained radiation oncologists,” says Dr. Mahantshetty. “I want to show them what’s possible. Because if it’s more exciting for trainee physicians, they’re more likely to take it up and we’ll see more patients benefit from it throughout the world.”
When you combine skills and technology, you’ll get the best of both – and that inevitably leads to better outcomes for patients.
Looking to the future of brachytherapy
A move to single room brachytherapy solutions could help a greater number of cancer patients throughout the world.
“I think more can be done to make treatments efficient and effective for both patients and clinicians,” concludes Dr. Mahantshetty. “By having the technology to carry out implantation, imaging and treatment in one room, we can optimize workflows, improve the patient experience and deliver better outcomes.”
Learn more about Elekta’s brachytherapy solutions.
LWBBX230107





