MR-only workflow is key to Spanish Center's approach to personalized, efficient radiation therapy


Synergy between Hospital La Paz’s Elekta Unity MR-Linac and Philips MR-simulator provides high-quality MR imaging and seamless MR-only workflows for prostate and rectal cancer patients
The advantages of MRI in radiation therapy – including more precise contouring, better targeting, margin reduction, and hypofractionation – are well-established, and new innovations and increased familiarity with MRI (e.g., via training) have reduced barriers to introduce MRI. Increasingly, institutions are also adopting MRI as the primary imaging modality in the entire radiation therapy workflow, eliminating the use of CT for both simulation and treatment. One of these centers is Hospital La Paz (Madrid, Spain). With two years of experience using MR-guided radiation therapy (MRgRT) with Elekta Unity, the hospital recently acquired Philips’ Ambition MR-RT. This MR-simulator not only offers exceptional soft tissue visualization but also provides CT-density information from a single MR acquisition, thus removing the need for CT-simulation. Hospital La Paz now exclusively uses MRI to treat their prostate and rectal cancer patients.
“With MRI we can better visualize the tumor and surrounding tissues compared to traditional CT and cone-beam CT during treatment, leading to more precise tumor delineation and minimizing radiation to healthy tissues.”
“One of the key advantages of MRI is its soft tissue visualization – both in diagnostic and MR-simulation scenarios,” says La Paz radiation oncologist Inmaculada Navarro, MD. “With MRI we can better visualize the tumor and surrounding tissues compared to traditional CT and cone-beam CT during treatment, leading to more precise tumor delineation and minimizing radiation to healthy tissues. And – thanks to real-time imaging and the ability to perform daily adaptive radiotherapy with Elekta Unity – we can reduce treatment margins, resulting in more focused treatments.”
Team confidently embraces MR workflow
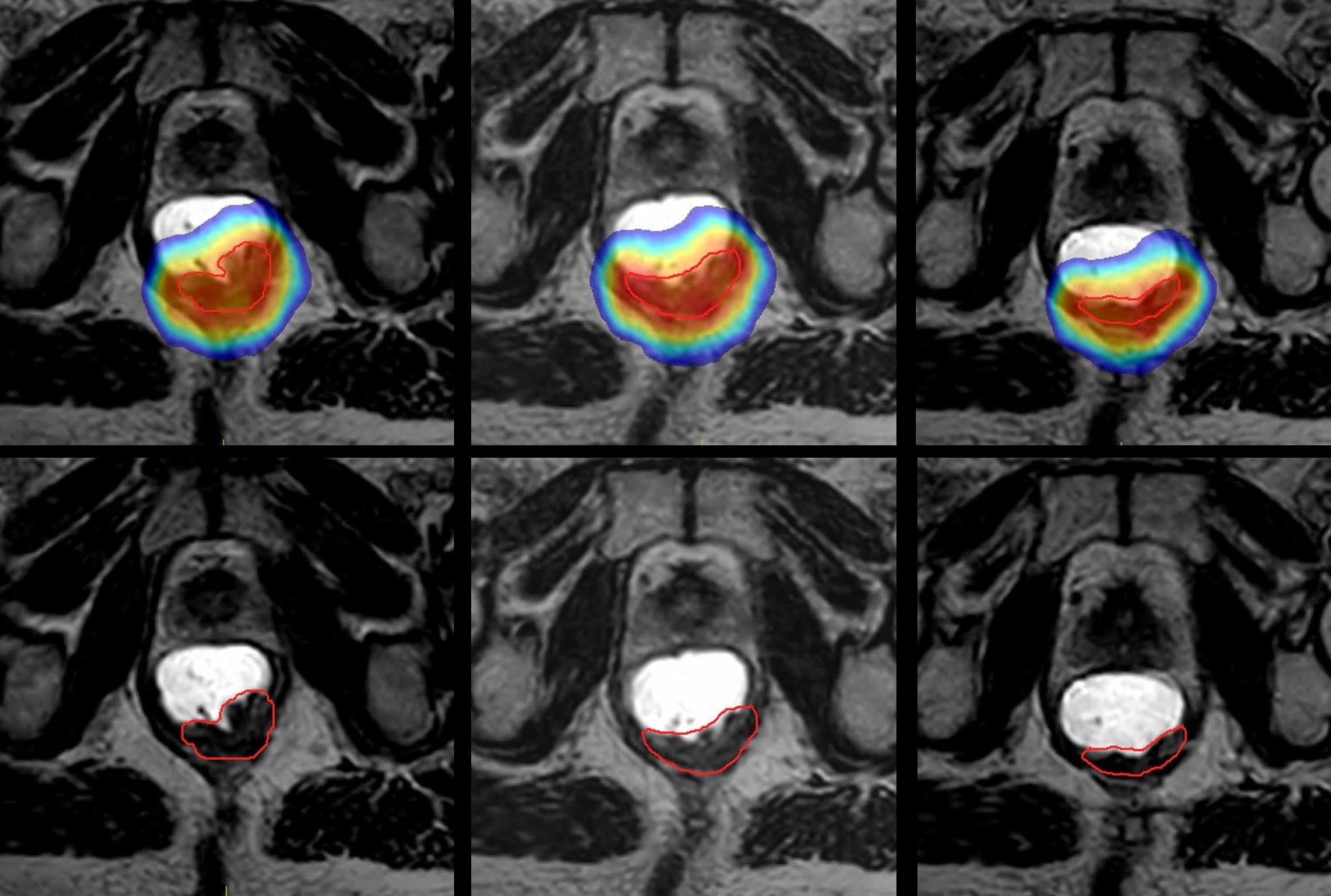
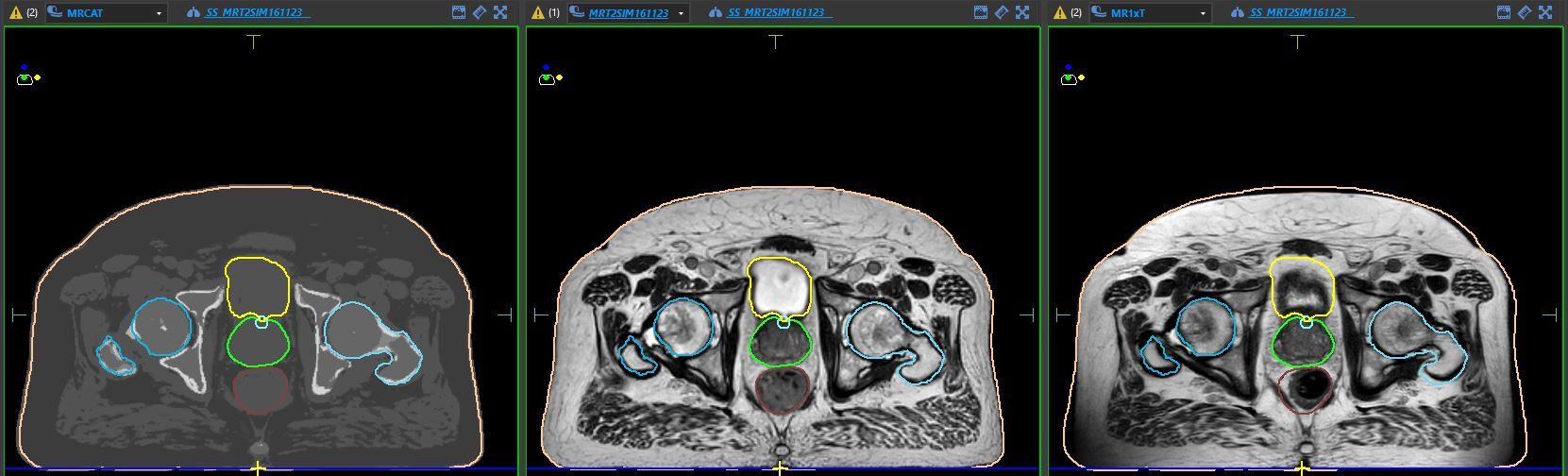
Since its clinical go-live, Hospital La Paz treats nearly all patients eligible for stereotactic body radiation therapy (SBRT) on Elekta Unity, especially those with tumors in the upper abdomen and pelvis where clinicians observe greater intrafraction or interfraction motion. Ninety-five percent of Unity treatments are SBRT or hypofractionated treatments with an average of seven fractions (Figures 1-2). All patients treated on Unity at Hospital La Paz undergo MRI simulation. Structures are delineated on the MR-sim and used to create the reference plan. At each treatment session, the reference plan is registered to the daily MR-Linac image, and the MR-delineated structures are propagated. This MR-MR registration decreases online planning time, requires fewer contouring corrections, and improves delineation accuracy compared to a CT-MR registration in which CT-delineated contours are used.1 (Figure 3).

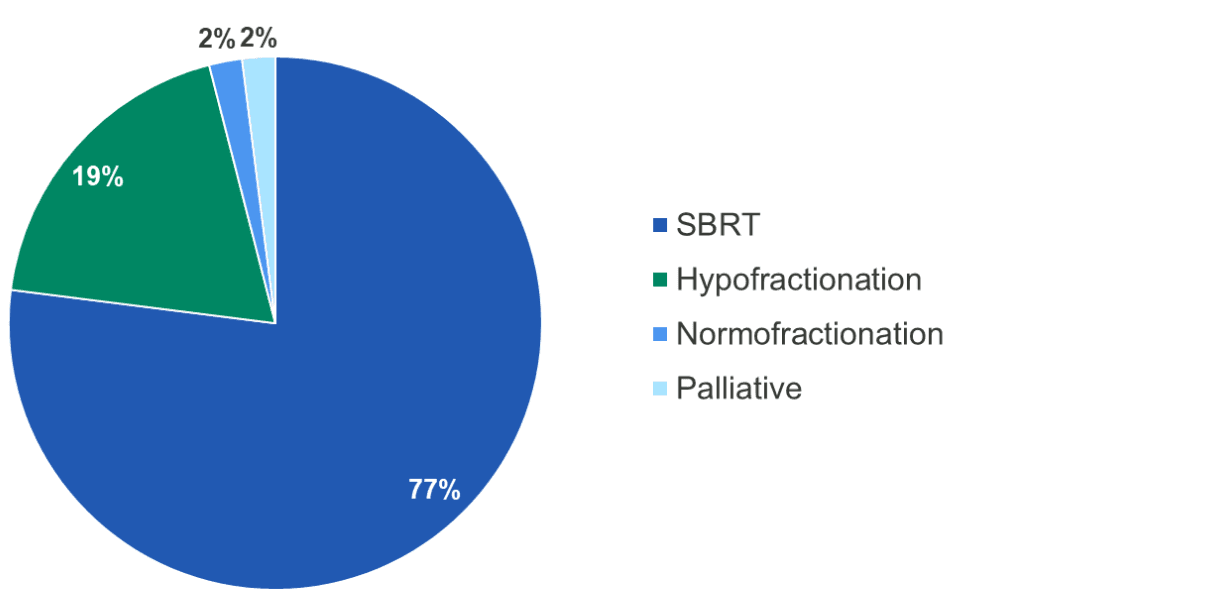
Figure 1 (left). Diagnoses treated with Unity. Figure 2 (right). Radiotherapy treatment schemes.
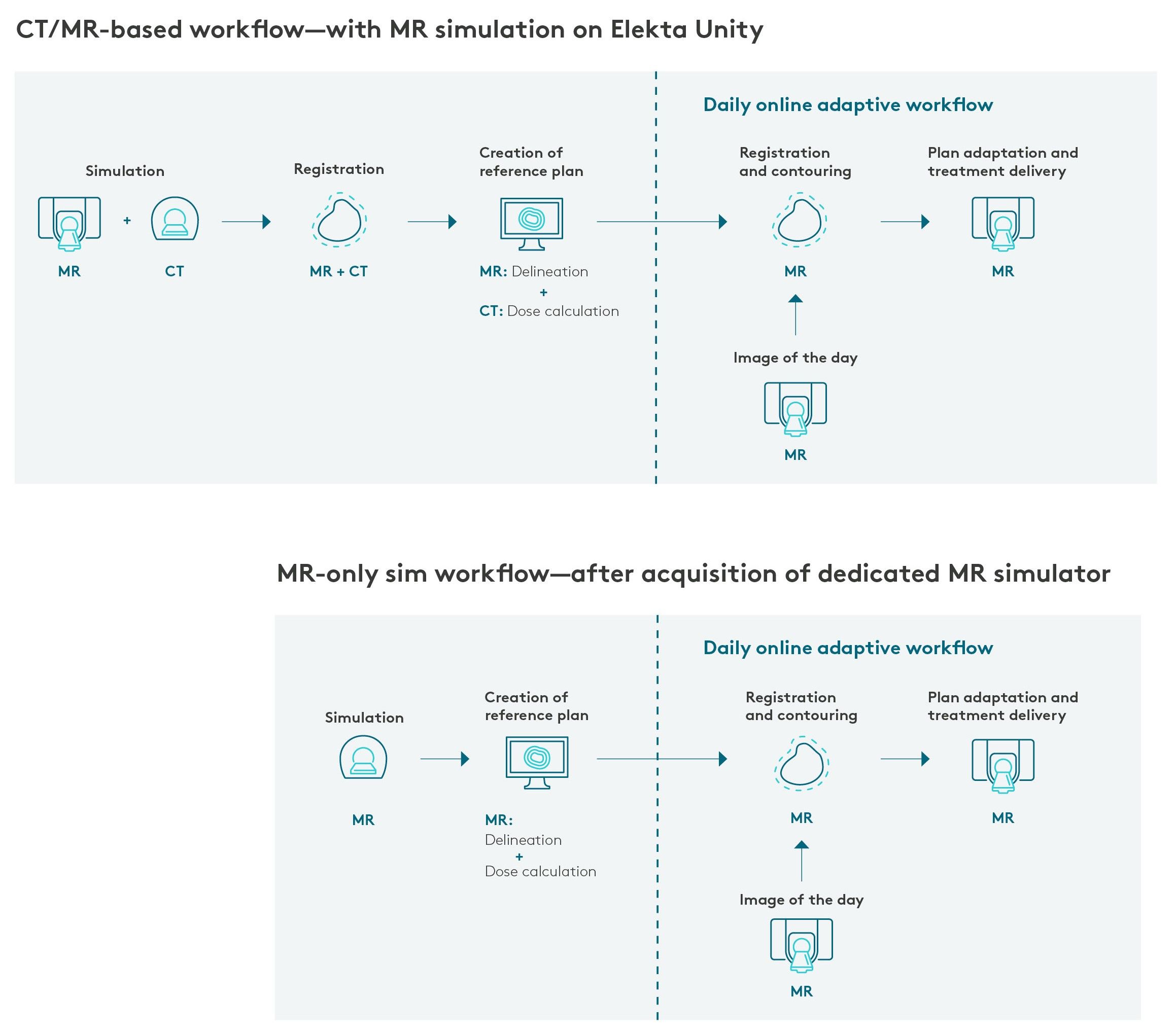
“Before we acquired a dedicated MR-simulator, all patients would be simulated on the MR-Linac to acquire multiparametric MR images for precise tumor delineation and to create an optimal reference plan for Unity,” Dr. Navarro says. “Patients were also scheduled for CT simulation, located at a 20-minute walk from the Unity facility, to acquire the necessary density information for dose calculation.
“Two separate appointments had to be scheduled for simulating patients who are Unity candidates, but we saw an opportunity to further streamline the MR-based workflow by implementing an MR-only simulation workflow and eliminate CT,” she adds.
Paving the way for a more efficient RT workflow
In 2023, the hospital had the opportunity to acquire a dedicated MR simulator and selected the Philips Ambition MR-RT. An important reason was that this system has the ability to generate MRCAT (MR for Calculating Attenuation) images to support an MR-only workflow and simulate patients in a single session.
“The Philips MR simulator – unlike a different vendor’s solution – provides a consistent patient setup and indexing with the same immobilization devices as Unity. This reduces setup errors, enhance treatment accuracy and minimize training requirements.”
“Philips Ambition 1.5T MR helps us simulate patients in a single session. Another advantage in day-to-day practice is that the Philips MR simulator – unlike a different vendor’s solution – also provides a consistent patient setup and indexing with the same immobilization devices as Unity,” Dr. Navarro observes. “This reduces setup errors, enhances treatment accuracy and minimizes training requirements. In addition, both systems provide similar, high-field image quality, which facilitates precise tumor delineation and informed decision-making throughout the treatment process. These synergies were anticipated to ultimately improve clinical efficiency and patient care.

“We also like the fact that we can easily exchange the Philips flat couch top with a diagnostic couch to enable the MR system to be leveraged for multiple uses,” she adds. “Therefore, the Philips MR-RT system’s location in the radiology department makes it shareable with other hospital specialties, such as radiology and cardiology.”
Installation of the MR-simulator was simplified by the Philips BlueSeal magnet, which doesn’t require a quench pipe. It also eliminated the concern regarding helium-related complications, as the cryostat is fully sealed and will never need a refill.*
A streamlined contouring and planning process with MR-only simulation
Expanding on the convenience, productivity and quality of contouring and planning with the Philips MR-RT/Elekta Unity combination, Dr. Navarro explains that by consolidating steps that previously required separate CT and MR imaging, the workflow is now faster and more efficient. In a traditional workflow, contouring the target area and organs-at-risk is often done separately on CT and MR images to capture different anatomical details.
“This can be time-consuming, as each image set needs to be aligned and reviewed by the medical team,” she says. “With an MR-only simulation workflow, we can perform all contouring on MRI alone.”
This provides several benefits, Dr. Navarro adds, including:
- Enhanced image quality for soft tissues: With MRI’s superior soft tissue contrast – particularly valuable in areas such as the pelvis – it allows more precise contouring of the target and surrounding organs without relying on additional CT images.
- Reduced times and resources: Consolidating contouring into a single MRI scan eliminates the need for dual imaging (CT and MRI), which reduces the time spent on image registration, alignment and verification.
- Increased patient comfort: Patients don’t have to schedule multiple appointments, translating to fewer trips to the hospital, less waiting time and a more streamlined treatment experience. All of these factors help alleviate stress and reduce time off of work or other obligations.
- Enhanced workflow and reduced wait times: By simplifying and streamlining the process, the department can optimize workflow, decrease scheduling bottlenecks, and ultimately reduce wait times for imaging and treatment planning. This allows La Paz staff to treat more patients with greater efficiency, thus improving both patient throughput and department productivity.
“An MR-only workflow allows us to maintain high accuracy in treatment planning, while improving the efficiency of the planning process, thereby enhancing both the patient experience and department operations.”

Before bringing MR-only simulation into clinical use the La Paz team went through a training (see sidebar) and commissioning process.
“Initially, we acquired the regular CT simulation and obtained MRCAT images from the MRI simulation. The physics team then created comparative radiotherapy plans for more than 30 patients using different sequences and compared the electron densities and Hounsfield units,” says La Paz medical physicist Carlos Ferrer. “Although the plans are not exactly identical, we found good agreement between the CT-based and MRCAT-based plans, giving us the confidence to use the MR-only simulation workflow for all pelvic patients. In a few cases, for example, in the presence of metallic implants or bone anomalies in elderly patients, we have encountered some issues with MRCAT image generation and electronic density assignation, meaning that not all patients will be candidates for this workflow.”
She adds that there is clinical evidence that MRCAT technology has been proven accurate for dose calculation.2-3 Combined with the hospital’s own internal validated data, this provided the confidence needed for the site to quickly adopt the MR-only workflow clinically.
By September 2024, Hospital La Paz had performed 286 treatments on Elekta Unity, with more than 20 of these planned and analyzed using the MR-only workflow.
“In summary, an MR-only workflow allows us to maintain high accuracy in treatment planning, while improving the efficiency of the planning process, thereby enhancing both the patient experience and department operations,” Dr. Navarro observes.
A view toward the future of MR in RT
“We are happy with our MR in RT program as it provides more personalized patient care,” she says. “We want to further expand our program to obtain MRCAT for brain and head-and-neck patients when we acquire suitable immobilizers. Once Comprehensive Motion Management [CMM] is implemented, we will include more patients with thoracic tumors, such as those requiring lung SBRT, to reduce margins.”
The future of MRI in radiation oncology holds considerable promise for improving treatment precision, enhancing patient outcomes and advancing the field of oncology, Dr. Navarro adds. “The increased use of functional MRI techniques – such as diffusion-weighted imaging and dynamic contrast-enhanced MRI – may become standard in radiotherapy,” she says. “These methods provide valuable information about tumor biology and response to treatment, thus enabling more informed decision-making.
“With advancements in MRI technology and software,” Dr. Navarro continues, “we can anticipate more efficient workflows that reduce the overall time for patients. This will enhance patient throughput while maintaining high quality care.”
Building proficiency in the MR-only MR-Linac workflow
To prepare staff for a MR-based workflow for Unity, Hospital La Paz had team members familiarize themselves on how to delineate targets and OARs with MRI.
“Once a certain level of proficiency with MRI has been achieved, we find it easier to delineate certain locations, especially soft tissues such as the prostate or the head of the pancreas, than with CT.”
“MRI-based contouring requires prior training in MR imaging and Unity workflows,” Dr. Navarro says. “Part of the team completed a training stay at an international center. We have also participated in Elekta conferences and courses to further our training. Currently, we have standardized the MRI sequences we use based on the type and location of the tumor. The radiation therapist specializes in contouring organs-at-risk, while the physicians focus on treatment targets, complex structures, and reviewing all contouring before planning. Currently, Hospital La Paz is a reference center for Unity training in Spain.
“In radiation oncology, treatment planning is usually done on CT images, for which the staff has greater expertise in contouring and planning,” she adds. “When starting simulation and treatment with MRI, the entire team, including physicians, radiation therapists and physicists must be familiar with different MRI pulse sequences and how tissues appear in each of them to accurately delineate and contour them. Once a certain level of proficiency with MRI has been achieved, we find it easier to delineate certain locations on MRI versus CT – especially soft tissues such as the prostate or the head of the pancreas, than with CT.”
Learn more about MRgRT with Elekta Unity.
*Even in the unlikely event that the magnet becomes unsealed, the negligible amount of helium escaping would not significantly affect the oxygen level within the room.
References
- Christiansen RL, Dysager L, Bertelsen AS, et al. Accuracy of automatic deformable structure propagation for high-field MRI guided prostate radiotherapy. Radiat Oncol. 2020 Feb 7;15(1):32. doi: 10.1186/s13014-020-1482-y. PMID: 32033574; PMCID: PMC7007657.
- Tyagi N, Zelefsky MJ, Wibmer A, et al. Clinical experience and workflow challenges with magnetic resonance-only radiation therapy simulation and planning for prostate cancer. Phys Imaging Radiat Oncol. 2020 Oct;16:43-49. doi: 10.1016/j.phro.2020.09.009. Epub 2020 Oct 13. PMID: 33134566; PMCID: PMC7598055.
- Kemppainen R, Suilamo S, Ranta I, et al. Assessment of dosimetric and positioning accuracy of a magnetic resonance imaging-only solution for external beam radiotherapy of pelvic anatomy. Phys Imaging Radiat Oncol. 2019 Jun 22;11:1-8. doi: 10.1016/j.phro.2019.06.001. PMID: 33458269; PMCID: PMC7807675.
LARMRL250311