MR-Linac Consortium meeting continues to expand MR-guided radiotherapy horizons

Elekta Unity users focus on building MRgRT clinical evidence base and streamlining workflow
The enthusiasm for MR-guided radiotherapy (MRgRT) continues to sweep across the globe, as new uses for the innovative treatment modality arise and as clinical evidence pours in, 1-10 as reflected at the 19th MR-Linac Consortium meeting in Singapore. The international meeting boasted 250 attendees from 20 countries representing 50 centers and featured more than 80 scientific presentations and workshops.
With the Consortium’s continued growth, the meeting has evolved to accommodate and leverage new members, with the 100th member site – Skåne University Hospital, which is based in Lund, Sweden – joining the global community of MRgRT enthusiasts.

New faces, clinical studies and workflow efficiencies highlighted
“The MR-Linac Consortium is continuously growing and stronger than ever, and the clinical evidence for MRgRT is rapidly growing as well,” says Cameron Baillie, Elekta Clinical Collaborations Lead, Medical Affairs and Clinical Research. “The Consortium is a vitally important forum for the global Elekta Unity community to partner and learn from each other.”
“This year, we introduced more breakout sessions and focus groups to cover a wide range of topics and to cater to diverse interests and expertise within the Consortium.”

“This year, we introduced more breakout sessions and focus groups to cover a wide range of topics and to cater to diverse interests and expertise within the Consortium,” he says. “We also organized enhanced networking opportunities, including interest group sessions and informal events to help members connect and collaborate more effectively.”
In addition, the MR-Linac Consortium meeting has incorporated more interactive formats, like panel discussions, workshops, and Q&A sessions to foster active participation and knowledge exchange, Baillie adds.
As in previous years, the MR-Linac Consortium named the best Clinical, Technical and Young Investigator abstracts. In 2024, the Consortium announced that two awards had been named after two of the community’s dedicated colleagues, with the Technical Abstract Award named after Elekta Unity pioneer Prof. Jan Lagendijk (University Medical Center Utrecht [UMC Utrecht], Netherlands) and the Clinical Abstract Award named after multi-year Consortium Chair Dr. Christopher Schultz (Froedtert & Medical College of Wisconsin, USA).
Dr. Pim Borman receives Young Investigator award

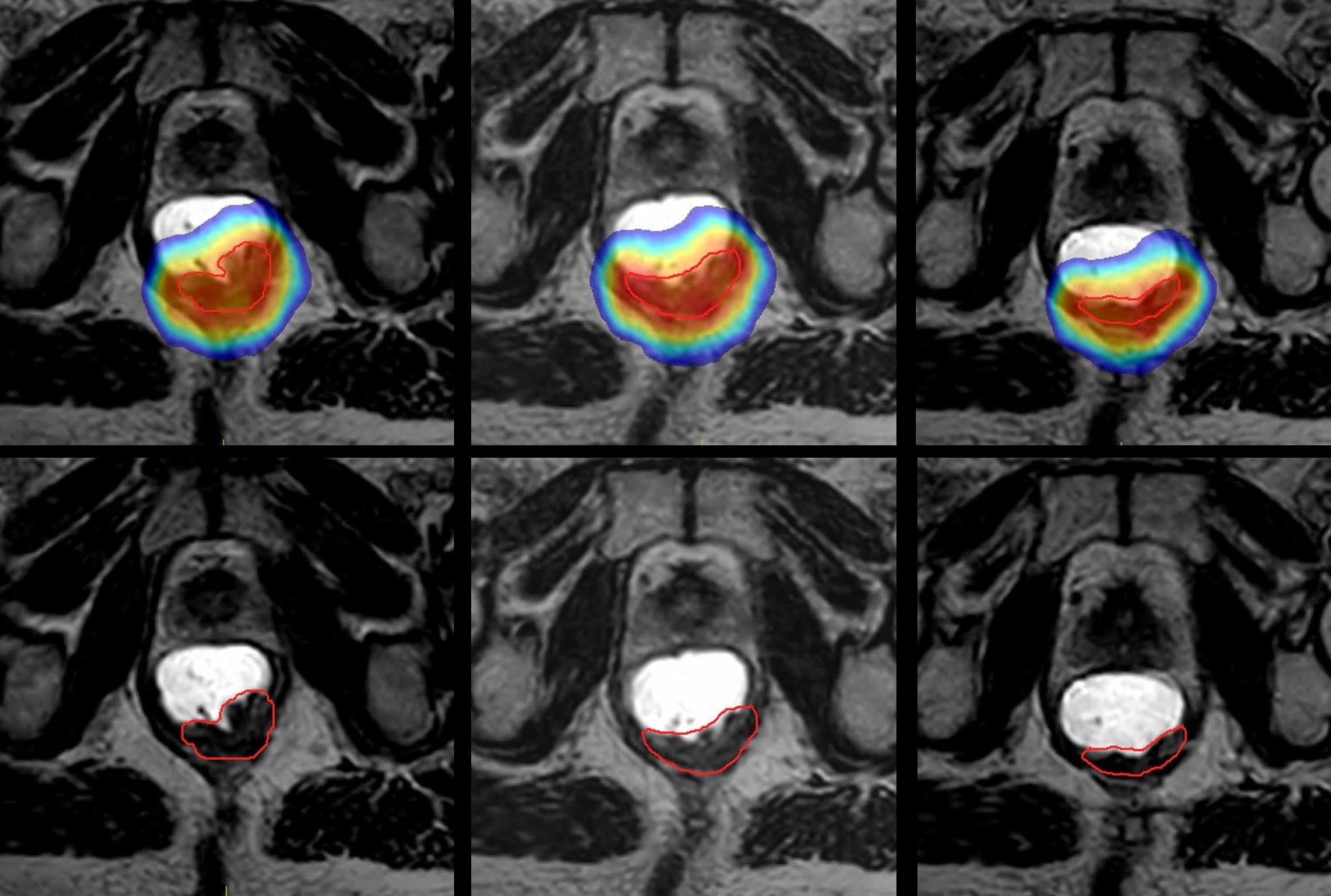
Pim Borman, PhD, Clinical Computer Scientist at UMC Utrecht presented on research integrating VMAT with MLC tracking on Elekta Unity, combining the efficient, precise dose delivery of VMAT with the MR-Linac’s exceptional soft tissue imaging for real-time dose delivery. 8 His team created and tested five VMAT plans for prostate, pancreas and liver cancers, recalculating the plans on a phantom to simulate patient conditions, and motion was introduced to test the system’s accuracy. Results showed that without MLC tracking, dose delivery was unacceptable, whereas with MLC tracking, the system achieved high accuracy and efficiency.
“This research is a good example of how the community is exploring ways to shorten treatment times, which we believe will accelerate widespread adoption of MRgRT,” Baillie says.
Dr. Daniel Palhares receives Schultz award
In his study, Daniel Palhares, MD, radiation oncologist at Sunnybrook Health Sciences Centre, investigated the use of diffusion-weighted imaging (DWI) to monitor apparent diffusion coefficient (ADC) changes in glioblastoma cellularity during radiotherapy. 1 ADC is lower in tumors with high cellular density, suggesting that regions of tumors resistant to chemoradiation would show smaller ADC reductions – indicating less drop in cellularity compared to responsive regions. A prospective study of 80 glioblastoma patients who underwent DWI at multiple points during and after chemoradiation compared ADC changes in tumor regions that later recurred versus those that didn’t. Results showed that resistant tumor regions had smaller ADC increases during therapy, suggesting that these areas were less responsive to therapy and more likely to recur.
“By using ADC changes to identify resistant tumor regions early in treatment, physicians can adapt therapy plans to target these areas more aggressively,” Baillie observes. “This approach could make radiotherapy more personalized and effective for glioblastoma patients.”
Maximilian Konrad earns Lagendijk Award
In a study of the feasibility and efficiency of AI-based delineation tools for daily Elekta Unity plan adaptation, Maximilian Konrad, PhD student at Odense University Hospital, and his team compared standard workflows with AI-assisted workflows in 10 prostate cancer treated over 10 sessions. The results demonstrated that AI-assisted workflows significantly reduced the delineation times throughout treatment, while also reducing inter-observer variability. The study concluded that implementing AI-assisted workflows is feasible and can improve the efficiency and consistency of radiotherapy planning, potentially enhancing daily treatment schedules and reducing delays.
“The implementation of AI-based delineation will reduce staff time spent on contouring and reduce overall treatment times.”
“The implementation of AI-based delineation will reduce staff time spent on contouring and reduce overall treatment times,” Baillie notes. Again, advancements like these are important to increase the overall efficiency of MRgRT treatments.”
Attendees reflect on the meeting’s value
His second MR-Linac meeting, medical physicist Jihun Kim, PhD (Gangnam Severance Hospital, Seoul, Korea), enjoyed the opportunity to network with and learn from other users. Gangnam Severance Hospital acquired Elekta Unity in 2021.

“The meeting also allowed me to make connections with others involved in MRgRT research,” Dr. Kim says. “For example, I met with users from Denmark who are doing research work on the clinical implementation of auto-segmentation for prostate cancer – which is similar to my investigations. There may be opportunities for collaboration with them.
“In addition, the MR-Linac meeting is unique among many other conferences in its singular focus on MRgRT as practiced by all the conference attendees,” he says. “We can have a very intense and concentrated meeting together.”
As a member of the Consortium’s biomarker brainstorm group, Dr. Kim found the abstract on the use of diffusion-weighted imaging (DWI) to explore treatment response in glioblastoma during radiation therapy particularly interesting. (see Schultz award above).
Radiation oncologist Sweet Ping Ng, MD (ONJCC Austin Health, Melbourne), notes that it was important that the MR-Linac Consortium meeting convened in an Asian country for the first time.

“Approximately 30 percent of the MR-Linacs are in Asia, which makes it vital to engage these Asia-Pacific institutions,” says Dr. Ng, an Elekta Unity user for the last three-and-half years.
She found the Hypothesis Testing Program (HTP) session particularly interesting.
“All the ideas presented were novel and they generated great discussions on new ways to utilize the MR-Linac for the best clinical care,” Dr. Ng says. “Overall, the conference was a fantastic opportunity to share ideas and data face-to-face with Unity users and with Elekta representatives.
“The meeting featured presentations not only from large academic institutions on new research findings, developments, the feasibility of novel imaging and treatment methods,” she adds, “but also those from private practices, which presented their insights on how to make MR-Linac workflows more efficient.”
Multiple touchpoints throughout the year
To stay engaged throughout the year, Consortium members have many touchpoints. In addition to regular meetings of the Tumor Site Groups, members can also take advantage of the monthly Consortium Knowledge Exchange webinar series. These webinars offer valuable insights sharing among users across three different areas: treatment planning, User Experience, and Education and Training.
“In addition, members can access our new members-only website, providing a comprehensive resource for ongoing collaboration,” Baillie says. “We also encourage members to get involved in Tumor Site, Brainstorm and Focus group activities, as well as the Hypothesis Testing Program. These tools and resources foster continues communication and knowledge sharing among Consortium members, thus enhancing collaborative expertise and collaboration.
References
- Palhares, DM, Lawrence, L, Soliman, H, et al. Early apparent diffusion coefficient (ADC) changes during concurrent chemoradiation (CRT): An imaging biomarker for recurrence prediction in glioblastoma. International Journal of Radiation Oncology*Biology*Physics. 120. e264. 10.1016/j.ijrobp.2024.07.590.
- Westley RL, Biscombe K, Dunlop A, et al. Interim toxicity analysis from the randomized HERMES trial of 2- and 5-fraction magnetic resonance imaging-guided adaptive prostate radiation therapy. Int J Radiat Oncol Biol Phys. 2024 Mar 1;118(3):682-687. doi: 10.1016/j.ijrobp.2023.09.032. Epub 2023 Sep 29. PMID: 37776979.
- Grimbergen G, Eijkelenkamp H, Snoeren LMW, Bahij R, Bernchou U, van der Bijl E, Heerkens HD, Binda S, Ng SSW, Bouchart C, Paquier Z, Brown K, Khor R, Chuter R, Freear L, Dunlop A, Mitchell RA, Erickson BA, Hall WA, Godoy Scripes P, Tyagi N, de Leon J, Tran C, Oh S, Renz P, Shessel A, Taylor E, Intven MPW, Meijer GJ. Treatment planning for MR-guided SBRT of pancreatic tumors on a 1.5 T MR-Linac: A global consensus protocol. Clin Transl Radiat Oncol. 2024 May 18;47:100797. doi: 10.1016/j.ctro.2024.100797. PMID: 38831754; PMCID: PMC11145226.
- Hassan SP, de Leon J, Batumalai V, et al. Magnetic resonance guided adaptive post prostatectomy radiotherapy: Accumulated dose comparison of different workflows. J Appl Clin Med Phys. 2024 Apr;25(4):e14253. doi: 10.1002/acm2.14253. Epub 2024 Feb 23. PMID: 38394627; PMCID: PMC11005979.
- Fink CA, Ristau J, Buchele S. et al. Stereotactic ultrahypofractionated MR-guided radiotherapy for localized prostate cancer – Acute toxicity and patient-reported outcomes in the prospective, multicenter SMILE phase II trial, Clin Transl Radiat Oncol, Volume 46, 2024, 100771, ISSN 2405-6308, https://doi.org/10.1016/j.ctro.2024.100771.
- Daamen LA, Westerhoff JM, Couwenberg AM, et al. Quality of life and clinical outcomes in rectal cancer patients treated on a 1.5T MR-Linac within the MOMENTUM study. Clin Transl Radiat Oncol. 2024 Jan 4;45:100721. doi: 10.1016/j.ctro.2023.100721. PMID: 38274389; PMCID: PMC10808928.
- Daamen LA, Westerhoff JM, Couwenberg AM, et al. Quality of life and clinical outcomes in rectal cancer patients treated on a 1.5T MR-Linac within the MOMENTUM study. Clin Transl Radiat Oncol. 2024 Jan 4;45:100721. doi: 10.1016/j.ctro.2023.100721. PMID: 38274389; PMCID: PMC10808928.
- Snyder JE, Fast MF, Uijtewaal P, et al. Enhancing delivery efficiency on the magnetic resonance-linac: A comprehensive evaluation of prostate stereotactic body radiation therapy using volumetric modulated arc therapy. Int J Radiat Oncol Biol Phys. 2024 Oct 26:S0360-3016(24)03520-X. doi: 10.1016/j.ijrobp.2024.10.028. Epub ahead of print. PMID: 39490905.
- Warda C, Gani C, Boeke S, et al. Simulation-free magnetic resonance-guided radiation therapy of prostate cancer. Phys Imaging Radiat Oncol. 2024 Nov 7;32:100667. doi: 10.1016/j.phro.2024.100667. PMID: 39624393; PMCID: PMC11609320.
- de Leon J, Jelen U, Carr M, et al. Adapting outside the box: Simulation-free MR-guided stereotactic ablative radiotherapy for prostate cancer. Radiother Oncol. 2024 Nov;200:110527. doi: 10.1016/j.radonc.2024.110527. Epub 2024 Sep 5. PMID: 39242030.
LARMRL241229