Forging a pathway to better cancer care for the LGBTQ+ community
While inequalities persist, driving an imperative to increase acceptance and improve practices
Lack of accessibility to world-class cancer care for LGBTQ+ individuals – like those in underserved areas around the world – remains a stubborn problem that many healthcare systems are striving to correct. In this community – beyond a scarcity of technology and trained personnel in certain regions – the challenges these cancer patients confront are systemic barriers to screening1, poor interactions with healthcare staff2, and inadequate training about this community in general, as well as transgender and non-binary people.3
In a bid to raise awareness about LGBTQ+ inclusive care among radiation therapy professionals, Stewart O'Callaghan, Founder and CEO of the patient-led LGBTIQ+ cancer charity, OUTpatients, along with therapeutic radiographers and hosts of the RadChat podcast, Naman Julka-Anderson and Joanna McNamara documented the inequalities these patients experience, in addition to their vulnerabilities for developing cancer in an ESTRO 2024 digital poster titled Person-centred through an LGBTIQ+ lens. O’Callaghan, a cancer patient and lead author of the paper, repeatedly sought LGBTQ+ support in multiple cancer centres over the years, only to be met with uncertain replies. This experience, among other factors, ultimately paved the way for the creation of OUTpatients.
“Despite the elevated prevalence of risk factors within this community, it remains essential that everyone have access to quality cancer care.”

“Despite the elevated prevalence of risk factors within this community, it remains essential that everyone have access to quality cancer care,” O'Callaghan says. “Notably, there also is a higher incidence of lung cancer among LGBTQ+ persons and this community shows a greater incidence of self-reported and rare GYN, skin, leukemia, bone and bladder cancers.”
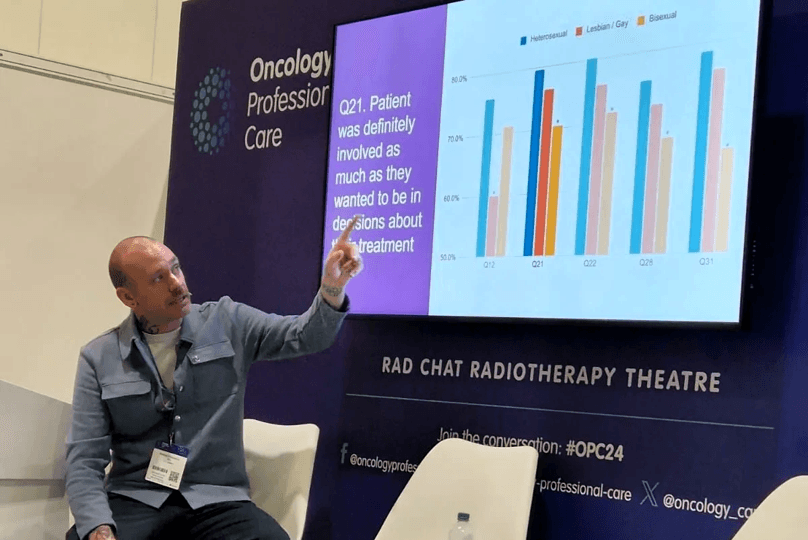
According to O'Callaghan, there seems to be a general insensitivity to the needs of LGBTQ+ cancer patients as measured by Cancer Patient Experience Survey (CPES) scores.4
“They feel like they don’t get enough information or support from caregivers or the ability to have family and other loved ones included during their cancer treatment journey,” continues O'Callaghan. “And nearly a quarter of these patients experience prejudiced comments, while almost 40 percent of trans individuals report undesirable patient-caregiver interactions as consequence of their gender identity.”
A notable aspect that is lacking in radiotherapy, are practices and procedures that are more inclusive, such as safer practices regarding pregnancy checks, O'Callaghan observes.
“While the IR(ME)R was updated in 2017 to be more encompassing in terms of gender diversity, the ambiguity of the procedures to follow – in at least one recorded case – led to a serious mistake,” continues O'Callaghan. “In this instance, a trans man had a CT while pregnant.”
Initiative designed to educate providers
To address this specific issue, the Society of Radiographers (SCoR) joined forces with UK radiographers and charities including OUTpatients. Their collaboration resulted in the creation of the 2021 Inclusive Pregnancy Status (IPS) Guidelines which aim to address healthcare inequalities in diagnostic imaging and radiotherapy, and help ensure transgender, non-binary and VSC/intersex patients receive safe and equitable cancer care.
“Being an LGBTQ+ person with cancer can feel isolating, so we want to equip professionals working in the cancer care sector with the knowledge and strategies they need to make their clinics more inclusive.”
“Being an LGBTQ+ person with cancer can feel isolating, so we want to equip professionals working in the cancer care sector with the knowledge and strategies they need to make their clinics more inclusive,” O'Callaghan says. “For example, we’ve designed a Provider Pack that offers core concepts for LGBTQ+ care, as well as supporting Cervical Screening Guidance for trans men and non-binary people with a cervix.”
Good results and areas of improvement identified
The trainings were well-received by many organizations and are frequently commissioned in London as the main content of a local training program. The webinars are now available online in the UK and earn over 95 percent scores on content and speakers, as well as on the likelihood that the training would affect practice.
“However, there has been sociopolitical resistance to its impact,” O'Callaghan says. “Some departments haven’t implemented the guidelines, citing among other things that the LGBTQ+ population is too small to warrant the work needed to implement them.”
“To achieve ‘patient-centered’ care, allyship and advocacy are needed at a greater scale with senior and institutional buy-in.”
O'Callaghan adds: “To achieve ‘patient-centered’ care, allyship and advocacy are needed at a greater scale with senior and institutional buy-in. The greater community needs to cooperate with LGBTQ+ organizations to jointly produce policies that foster inclusive practices and lead to improved pathways for patients experiencing barriers or exclusion – there is no better time to start than now.”
In a related article, Elekta spoke to oncologist Dr. Dan Saunders on the unique needs and concerns of LGBTQ+ patients with cancer and what he believes can be done to improve disparities. Click here to read.
LARNPS240612
References
- Haviland KS, Swette S, Kelechi T, et al. Barriers and Facilitators to Cancer Screening Among LGBTQ Individuals With Cancer. Oncol Nurs Forum. 2020 Jan 1;47(1):44-55. doi: 10.1188/20.ONF.44-55. PMID: 31845916; PMCID: PMC7573971.
- https://www.leeds.ac.uk/news-health/news/article/4005/report-highlights-experiences-of-lesbian-gay-and-bisexual-people-with-cancer
- https://www.cancer.gov/news-events/cancer-currents-blog/2024/cancer-care-challenges-lgbtq-plus-people
- https://www.ncpes.co.uk/