Active Breathing Coordinator streamlines treatment for several indications at Indian clinic
Patient-directed respiratory motion management system improves tumor targeting precision, reducing radiation exposure to healthy tissues
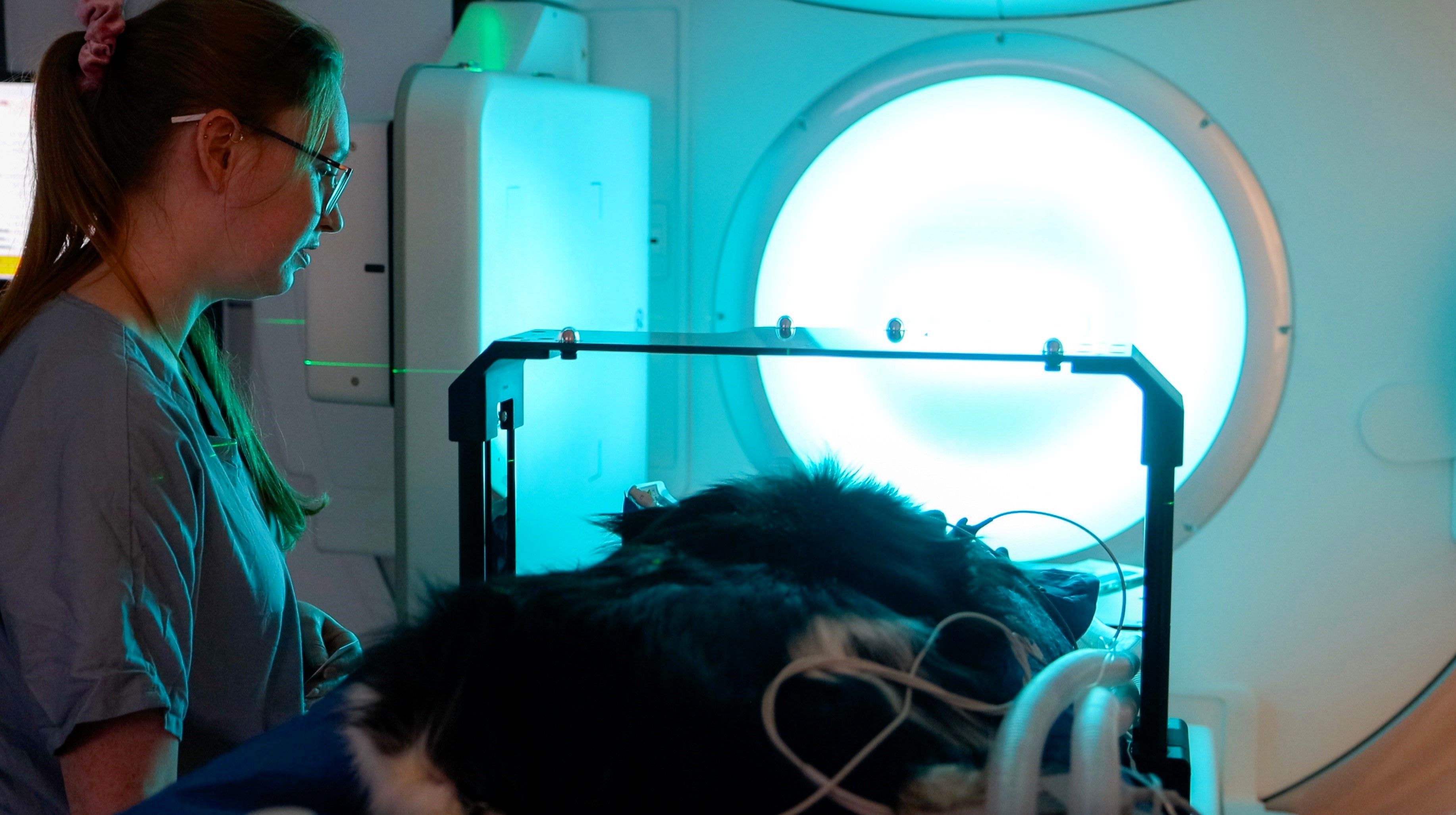
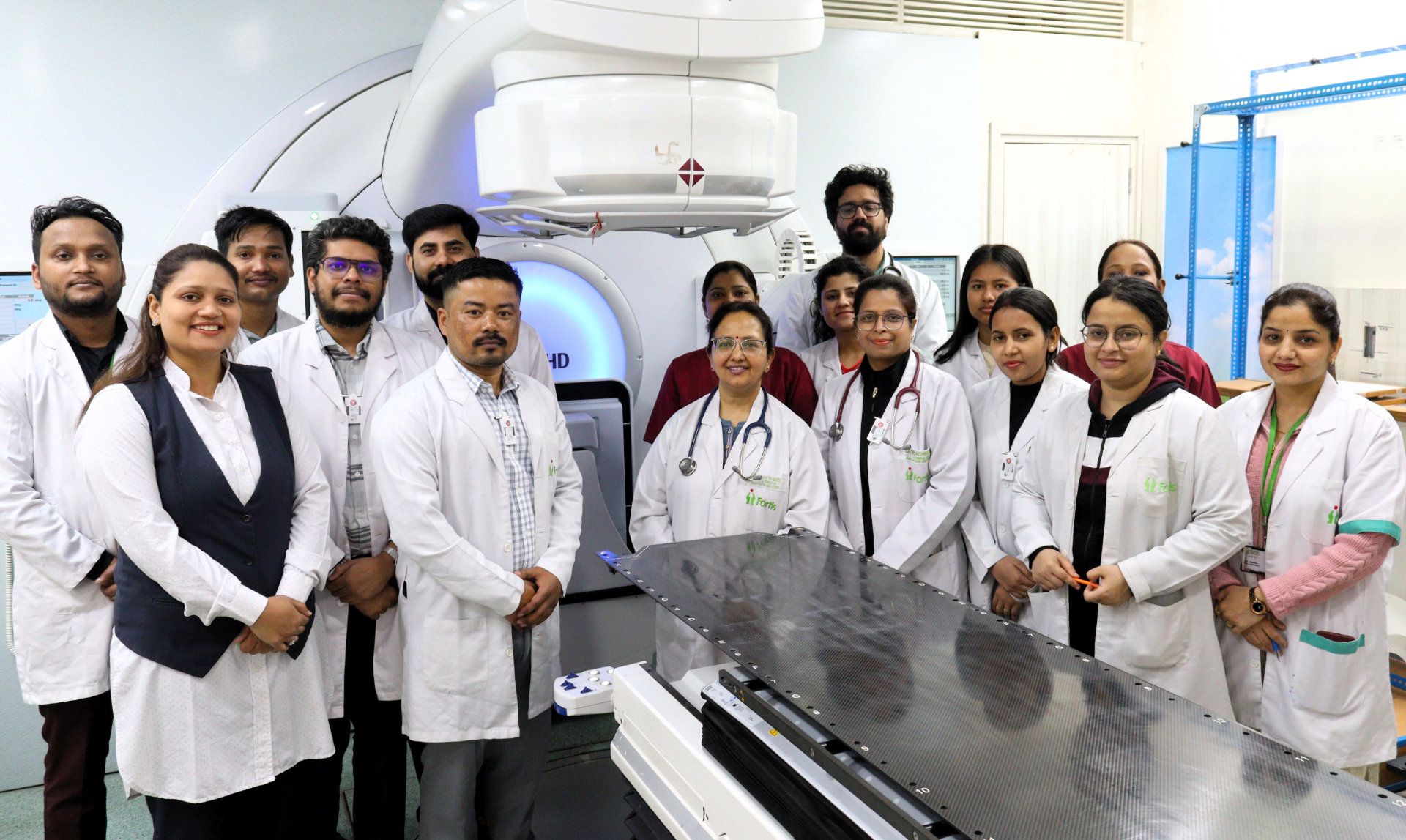
Auxiliary radiation therapy equipment rarely shares the spotlight but at Fortis Hospital, Shalimar Bagh (Delhi, India), Elekta’s Active Breathing Coordinator™ (ABC) has proven to be the exception. For the last three-and-a-half years, Fortis radiation oncologists have been using ABC (see sidebar) to simplify respiratory motion management for the treatment of patients with a variety of cancers – breast malignancies especially – and its benefits in a supporting role have not gone unnoticed among Fortis’s radiation oncology team.
“My colleagues and I find ABC to be a very robust, patient-friendly system, and the patient treatment setup using ABC very reproducible.”

“I have always been passionate about treating breast cancer patients with breath-hold based radiation therapy. My colleagues and I find ABC to be a very robust, patient-friendly system, and the patient treatment setup using ABC very reproducible,” says Vineeta Goel, MD, Fortis Hospital’s Senior Director & Head of Radiation Oncology. The hospital acquired Elekta’s Versa HD™ linear accelerator, Flexitron® brachytherapy afterloader and ABC in 2017. “In addition to breast cases, we use ABC for various other situations and indications.”
Fortis Hospital treats an average of 35 patients each 11-hour day on its Versa HD linac.
Simple patient training
According to Dr. Goel, voluntary breath holding without using ABC is quite difficult and non-reproducible during everyday treatment.
“Most patients don’t feel that ABC is challenging to train on – their experience has been phenomenal.”
“If I was training 10 women, only seven would be trained enough to do the treatment using voluntary DIBH for breast cancer radiation therapy,” Dr. Goel says. “Conversely, with ABC the patient training success is as high as 95 to 97 percent. Most patients don’t feel that ABC is challenging to train on – their experience has been phenomenal.
“We take 25 to 30 minutes on average for breast cancer treatment with ABC, she continues. “So, yes, ABC does increase treatment time, but it is absolutely worth spending extra time on the machine, as it improves radiation plan quality and critical organ safety for patient.”
She emphasizes that both Fortis staff and patients were concerned about switching from the voluntary respiratory motion management system to ABC.
“I thought patients would find the mouthpiece and nose clip very claustrophobic,” Dr. Goel observes. “On the contrary, we have found that virtually no one complained. Also, compared to the former system – because it was voluntary breath holding as the treatment proceeds – the patients tended to get exhausted, and reproducibility was never a straight line of breath holding. ABC’s spirometer, however, is constantly helping patients hold their breath – the breath holding that we can achieve is far better.”

It’s not just training and execution that have improved, according to Dr. Goel.
“When I look at their cone beam CTs, I am filled with satisfaction and pride. With the first CBCTs I saw the matching was so perfect that it was hard to believe,” she says. “I was not getting that kind of perfection with voluntary DIBH. Consequently, we gradually extended ABC to more indications.”
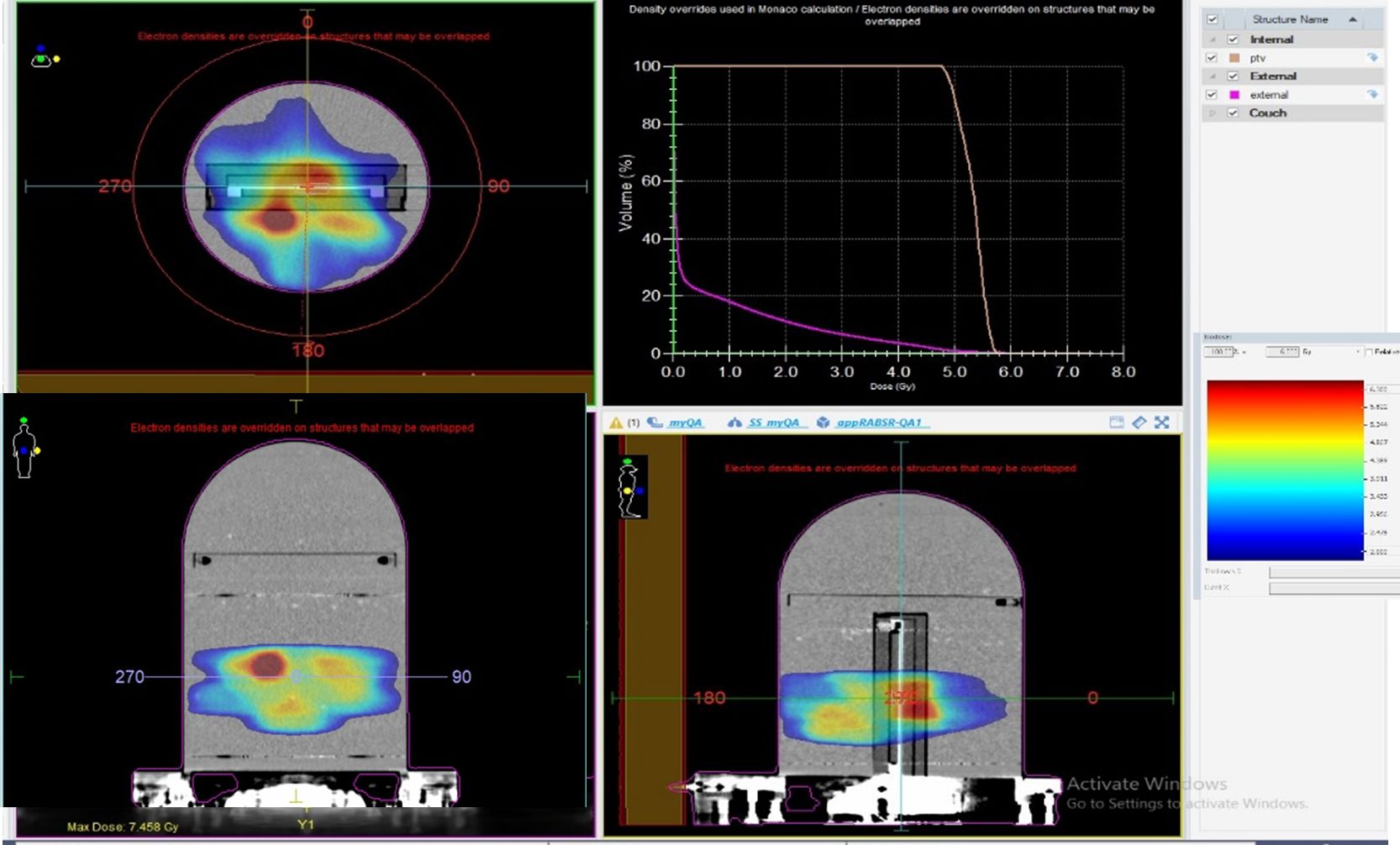
Regarding margins for ABC versus non-ABC, for breast cancer patients the margins are the same.
“However, there is a significant reduction in margins when we do SBRT lung, liver, pancreas, and lymph nodes without ABC, Dr. Goel notes. “Our practice is to do SBRT to these sites with ABC as far as possible. Our margins reduce by 60 to 70 percent with the use of ABC.
“We feel more comfortable and confident reducing margins with ABC,” she adds. “The system is a very robust, patient-friendly solution for freezing organ motion.”
Diverse uses for ABC
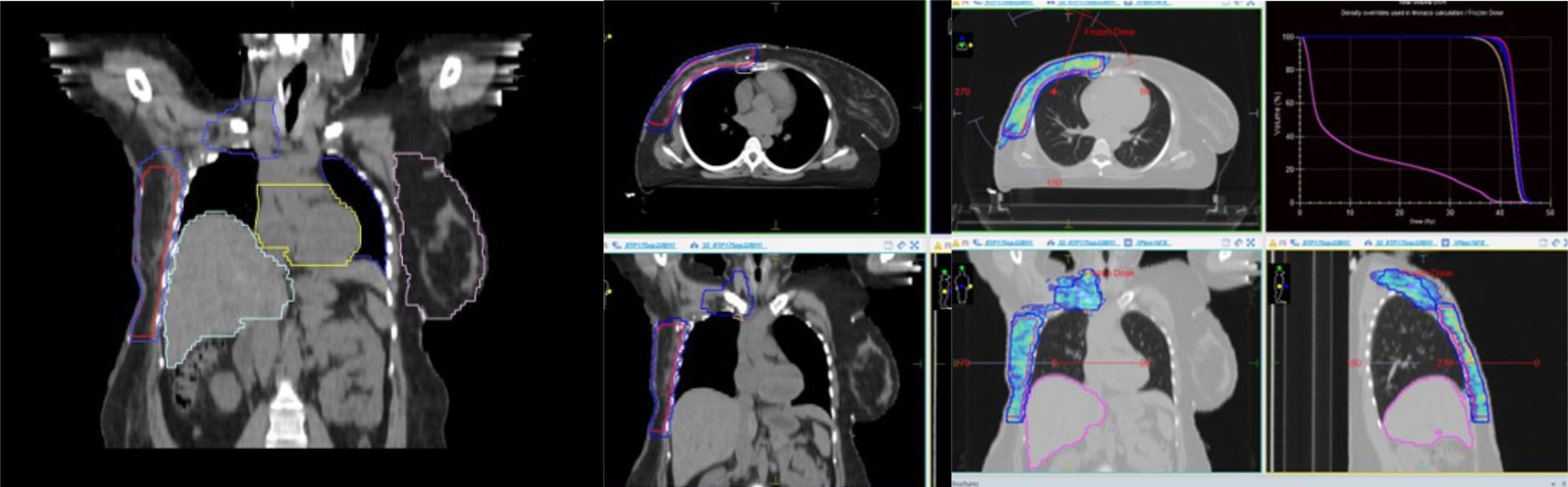
In addition to right- and left-sided breast cancer, Fortis clinicians have employed ABC for primary and metastatic lung cancers, as well as liver and adrenal metastases, esophageal malignancies and rare indications, such as Ewing sarcoma of pleura.
In a recent case of advanced esophageal cancer in a young patient, Dr. Goel recalls that she was finding it difficult to achieve a suitable lung dose.
“We wanted to give him radical radiation therapy to the bilateral supraclavicular fossa and the entire esophagus,” she says. “That was when I decided to use ABC to expand the lung volume and decrease the ITV toward the heart.”
Another young pregnant patient with right-sided breast cancer had received chemotherapy and surgery before delivering her baby. She subsequently came to the radiation therapy department for further treatment.
“Post-pregnancy the patient had gained a lot of weight, so when I took a radiation planning scan because of that weight gain, her liver had moved quite a bit cranially, which made the right lung volume very small,” Dr. Goel explains. “We put her on ABC, which helped us reduce both her lung and liver doses.”
“With ABC it’s possible to use non-coplanar beams.”
“At times, we also do intrafraction imaging,” she adds. “In addition, with ABC it’s possible to use non-coplanar beams. The previous motion management system comprised a stationary camera mounted on the ceiling, such that if we moved the patient support the reflective box on the patient’s chest the box can’t be seen and thus the position becomes inaccurate. With ABC, now at least we are able to use some angulations if they’re required.”
For an eight years-old child with Ewing sarcoma, Fortis clinicians had to irradiate his entire left pleural margin, volumes similar to as one would deliver for a patient with mesothelioma. However, since the boy was 8 years old his lung volume was very small at just 450 cc’s.
“I was required to give a dose of 45 to 50 Gray,” she recounts. “We taught him how to use ABC, the ITV reduced and the lung volume expanded and we could safely treat entire pleura while protecting lung parenchyma.”
At the other end of the age spectrum, an 82-year-old male patient had a tiny lung metastasis at a “very peculiar” location, according to Dr. Goel. It was at the junction of the heart, lung, liver and esophagus.
“To deliver lung SBRT for the met, I wanted to avoid the ITV and keep the volume minimal,” she says. “I was pleased that even at his age, he was able to train on ABC to successfully treat the lesion.”
Treatment times across all indications average 30 minutes.
Next up for ABC respiratory motion management
With the success of ABC for a variety of indications, Dr. Goel and her colleagues are looking forward to trying the system for new uses.
“We have yet to employ ABC for a renal SBRT case,” she says, “but whenever we get a suitable patient, we have already done our background homework and are eager to try it for that indication.”
What is Active Breathing Coordinator?
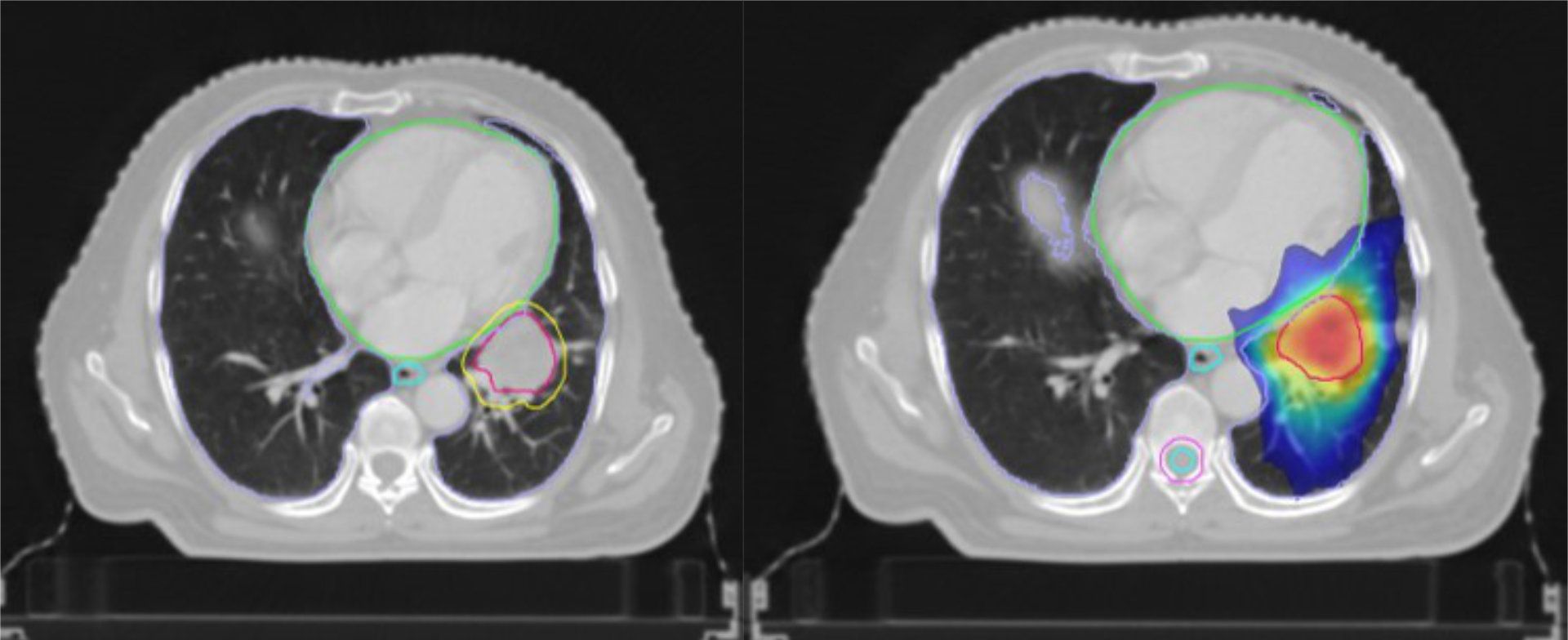
To manage respiratory motion, Elekta’s Active Breathing Coordinator (ABC) uses a spirometer to monitor the patient’s breathing cycle in real time by tracking the respiratory cycle, thereby providing the patient’s lung volume and airflow. The system detects when the patient reaches specific points in their breathing pattern – typically at full inspiration – and prompts them to hold their breath. This breath-hold technique temporarily stops lung or abdominal motion, enabling precise radiation beam delivery to the tumor.

The system’s real-time monitoring ensures that radiation is delivered only when the tumor is in the optimal position, thus minimizing exposure to healthy adjacent tissues. By synchronizing radiation delivery with the patient’s breathing cycle, ABC decreases treatment-related side effects and enhances treatment outcomes, especially for tumors in areas prone to respiratory motion, such as the lungs and liver.
Click here to learn more about Elekta’s motion management technologies.
LAROX250225